Wound Care
Tissue/cell types
Slough – yellowish soft foo of non-viable dead skin cells, fibrin, depris – breeding ground for bacteria
Granulation tissue – healthy red granular tissue in late stages of
HEALING – new blood vessels and connective tissue
Epithelial tissue – healthy along edges of dealing wound <- risk for maceration
Nectroic tissue
?Fibrous tissue; adipose and muscle

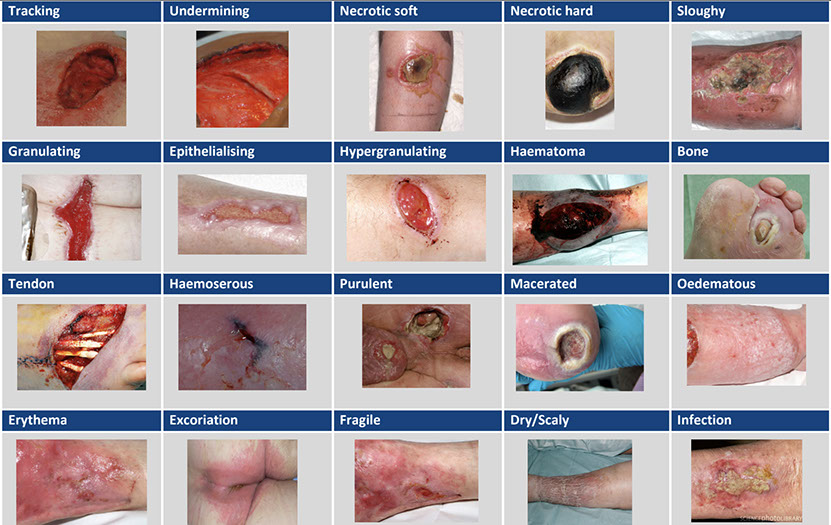
Tissue wound types [1]
Wound stages and treatments
Stage 1
Turn
Skin barrier cream:
- (kalmozine) zinc oxide cream
- A&D (soothe and cool moisture barrier) Vaseline white petroleum jelly
A+D+aloe
- Z-guard paste – combo of above with zinc oxide and petroleum
– makes it more slippy
Also helps with moisture incontinence
Tegaderm (cheap)
Optifoam (cheap) – edges curl – more for stage 2 or when drainage
This may be better for heals
Stage 2, skin tear
Duoderm (cheap) (hydrocolloidal) dressing (apple pectin) – may stick to bedding
vs adaptic (medium$ but can be left on longer) – non-adhering dressing – mesh+petroleum
Foam dressing (if wet) to absorb +/- silver (expensive, 2-3 weeks max due to resistence)
Little drain? – hydrogel (medium$) – for super dry stage 2 wounds
Medi-honey for bigger stage 2t
Hydroguard $? (silicone cream) – creates a ‘film’ apply to EDGES of wound to prevent maceration at edges. Also for around ostomies
ALWAYS wound cleanser – has surfactant – kills microbes – better than saline
Dressing change frequency
Stage 2 couple times a week
Barrier cream whenever wet diaper
Stage 3
Hydrogel with silver
Honey
calcium alginate
Foam dressing with silver
Silver no more than 3 weeks, microbes become resistant
Silvasorb gel
Therahoney gel
Calcium alginate (medium$) dressing or gel absorbs exudate so bed can heal – need to irrigate gel out after use – get wound bed to move ‘up’
+
Gauze or kerlix to soak extra fluid
Heavy discharge/infected wounds – MeSalt (cheap) – helps break necrotic tissue (rope dressing like calcium alginate) absorbs A LOT
Rope for packing, leave some sticking out always. Use if expecting healing.
Iodoform (medium$) – ribbon of gauze with iodine – when poor prognosis
‘xeroform’ (medium$) is a brand that comes with Vaseline imbedded compound
‘nu-guaze’ (cheap) also similar to above without iodine (if no sign of infection)
PuraCol (expensive) + 100% collagen, diabetic ulcers, burns, vascular ulcers. Natural wound environment.
Heal from bottom up – pack.
Pack with soaked dressing – ‘wet to dry’
Slough wound bed (non-viable, non-granulating)
Dressing change frequency
Stage 3 depends frequency
Stage 4
Try MeSalt and loads of gauze – absorbs exudate and creates moist environment NaCl helps break dead tissue and antimicrobial
Anything else?
Not going to heal
Dressing change frequency
Stage 4 packing – daily
Foley for wound protection
Unstageable
Santyl (expensive and inefficient) – brand name – break down necrotic tissue but so will medihoney if left long enough – very expensive
DTI
Not much to do until open. Barrier cream to help prevent opening.
Misc
Debridement kit – scalpel, scissors
Big thick eschar – ‘score’ it with little cuts
Non-arterial leg wounds (venous) – coloflex compression bandage
First layer is like calmoseptine and then compression wrap – both come in package
Medfix – adhesive tape – hypoallergenic tape
Barrier cream whenever wet diaper
'Afrin for bleeding wounds.
If dry wet it, if wet dry it.
Flagyl for wounds that smell.
Anti-fungal (clear moisture barrier with antifungal) – alternative to flagyl
See medline wound care pocket guide
Decision Tree for Lower Extremity Wound Care
1. **Assess the Wound**
- **Type of Wound**: Determine if it's a laceration, ulcer, abrasion, burn, etc.
- **Wound Depth**: Superficial, partial-thickness, full-thickness.
- **Wound Size**: Measure the length, width, and depth.
- **Exudate Level**: None, low, moderate, high.
- **Infection Signs**: Redness, warmth, swelling, pus, foul odor.
2. **Clean the Wound**
- **Remove Debris**: Use saline solution or sterile water.
- **Disinfect**: Apply antiseptic solution if necessary.
3. **Evaluate for Debridement**
- **Necrotic Tissue**: If present, consider debridement (mechanical, enzymatic, or surgical).
4. **Choose Initial Dressing**
- **Low Exudate**:
- Use non-adherent dressing (e.g., Telfa) with a secondary dressing.
- **Moderate Exudate**:
- Use hydrocolloid or foam dressing to manage moisture.
- **High Exudate**:
- Use alginate, super absorbent, or foam dressing to absorb excess fluid.
5. **Assess for Infection**
- **Signs of Infection Present**:
- Apply an antimicrobial dressing (e.g., silver, glycerin, manuka honey, iodine) and consult a
healthcare provider.
- **No Infection**:
- Continue with the selected dressing and monitor regularly.
6. **Monitor and Reassess**
- **Daily or Weekly Checks**: Depending on wound severity and healing progress.
- **Adjust Dressing Type**: Based on changes in exudate levels, wound size, and signs of
infection.
7. **Consider Advanced Dressings (If No Improvement) **
- **Evaluate Healing Progress**: If no significant improvement after 2-4 weeks. (see LCD)
- **Consult Wound Care Specialist**: For potential use of amniotic membrane dressings.
8. **Implement Advanced Dressing**
- **Preparation**: Ensure the wound bed is clean and free of infection.
- **Application**: Follow specific instructions for amniotic membrane dressing use.
- **Monitor**: Continue regular assessment and adjust as needed.
This decision tree provides a structured approach to wound care, emphasizing initial assessment
and basic wound management before considering advanced treatments like amniotic membrane
dressings.
Dressing categories:
Wound care dressings can be categorized based on their properties and the type of wound they are
designed to treat. Here are the primary categories:
1. **Gauze Dressings**
- **Properties**: Absorbent, available in sterile and non-sterile forms, can be impregnated with
various substances.
- **Use**: Basic wound coverage, primary or secondary dressing, packing for deep wounds.
2. **Non-Adherent Dressings**
- **Properties**: Do not stick to the wound bed, minimizes trauma during dressing changes.
- **Use**: Superficial wounds, minor burns, abrasions, and donor sites.
3. **Hydrocolloid Dressings**
- **Properties**: Occlusive, forms a gel in contact with wound exudate, maintains a moist
environment.
- **Use**: Partial and full-thickness wounds, pressure ulcers, minor burns, and venous ulcers.
4. **Hydrogel Dressings**
- **Properties**: High water content, provides moisture, can cool and soothe wounds.
- **Use**: Dry or minimally exuding wounds, burns, necrotic wounds, painful wounds.
5. **Foam Dressings**
- **Properties**: Highly absorbent, provides cushioning and protection, semi-permeable.
- **Use**: Moderate to heavily exuding wounds, pressure ulcers, leg ulcers, surgical wounds.
6. **Alginate Dressings**
- **Properties**: Derived from seaweed, highly absorbent, forms a gel when in contact with
exudate.
- **Use**: Moderate to heavily exuding wounds, cavity wounds, venous ulcers.
7. **Film Dressings**
- **Properties**: Transparent, adhesive, waterproof, allows oxygen exchange.
- **Use**: Superficial wounds, minor burns, as a secondary dressing, protection of IV sites.
8. **Composite Dressings**
- **Properties**: Combination of different dressing types often includes a non-adherent layer,
absorbent layer, and adhesive border.
- **Use**: Various wound types, moderate to heavy exudate, surgical wounds.
9. **Antimicrobial Dressings**
- **Properties**: Contain agents like silver, iodine, or honey, designed to reduce bacterial load.
- **Use**: Infected wounds, wounds at high risk of infection.
10. **Hydrofiber Dressings**
- **Properties**: Highly absorbent, converts to gel upon absorbing exudate, maintains moist
environment.
- **Use**: Moderate to heavily exuding wounds, cavity wounds, leg ulcers.
11. **Collagen Dressings**
- **Properties**: Promote wound healing by providing a scaffold for new tissue growth.
- **Use**: Chronic wounds, pressure ulcers, surgical wounds.
12. **Amniotic Membrane Dressings**
- **Properties**: Derived from human amniotic membrane, contains growth factors and
extracellular matrix components.
- **Use**: Chronic wounds, burns, surgical wounds, diabetic foot ulcers.
References:
1. Healthcare improve Scotland.
https://archive.healthcareimprovementscotland.scot/www.healthcareimprovementscotland.org/our_work/patient_safety/tissue_viability
Also see:
Scottish Wound Assessment and Action Guide:
https://drive.google.com/file/d/1-hC-93IYQp3jM4sE6JvTY6sJFYIv-SOH/view
Grey J. Wound Assessment:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1360405/
XWrap
https://www.appliedbiologics.com/product-showcase/xwrap-ecm/
Website for free wound care education and tools:
www.nmwoundcare.com
