Vulva and Vagina
Anatomy / Embryology
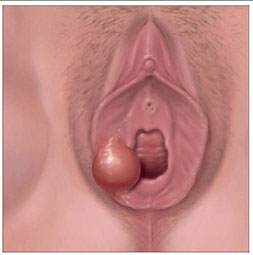
Bartholin cyst
Cysts
Condyloma acumulatum
Lichen sclerosus
Squamous hyperplasia
Vulvar fibroepithelial polyps
Vulvar Squamous Papilloma
Extramammary Paget disease of vulva
Vaginal Intraepithelial Neoplasia (VaIN)
Vulvar Intraepithelial Neoplasia (VIN)
Superficially Invasive Squamous Cell Carcinoma (SISCCA)
Angiomyofibroblastoma
(Aggressive) Angiomyxoma
Clear cell adenocarcinoma (CCA) of vagina
Granular cell tumor
Vulvo-vagina
Anatomy / Embryology
The urogenital sinus is formed when the cloaca is divided by the urogenital septum
- will eventually become the lower part of the vagina and the vestibule of the external genitalia
- superiorly come in contact with the mullerian ducts, which form the upper part of the vagina, the cervix, uterus and fallopian tubes
- the ovaries are formed from a structure attached to the mesonephros and mesonephric duct
-- the mesonephric (wolffian) ducts normally regress in adults, but remanants can be found esp in the mesovarium (the broad ligament) or along the lateral portion of the uterus, and may form Gartner duct cysts

Cysts
Includes: endometriotic cyst, follicular (epidermoid) cysts, steatocystoma multiplex, Bartholin cyst, mucinous cyst, mesonephric (Gartner) cyst, mullerian (endocervical type), ciliated cyst, paraurethral (skene) gland cyst,
Batholin cyst
Bartholin gland blockage from acute inflam of Bartholin gland (adenitis), usually in women over 40 yo
- can form abscess c std's
- can grow up to 5 cm or more, causing pain
Micro: squamous or transitional (urothelium) epithelium common
-- can see mucosal glands
-- may have malakoplakia
Tx: excise or marsupialized
Endometriotic Cyst
Bartholin cyst
Follicular (epidermoid) cyst
Dilation of hair follicle epithelium
- micro: usually dilated infundibulum, c a granular layer filled c loosely packed keratin (like an EIC)
Steatocystoma multiplex
Dominant inherintance, widespread, multiple, thin-walled cysts of skin, lined by squames and sebaceous cell lobules
- micro: collapsed cyst c sebaceous units in wall c intricate folding, thin stratified squames lined thin strongly eosinophilic cuticle lacking a granular layer
Mesonephric (Gartner) cyst
Cuboidal epithelium, would expect on a 3 or 9'o'clock bx along lateral vag wall where mesonephric duct was
(+) CD10
- only very rarely become malig

Gartner (mesonephric) cyst
Paraurethral (skene) gland cyst
Female homologue of male prostate gland, found on both sides of the urethral meatus
- probably derived from ducts and not acini
- Micro: lined by transitional or squames on a BM, c rare luminal cells c intracytoplasmic mucin
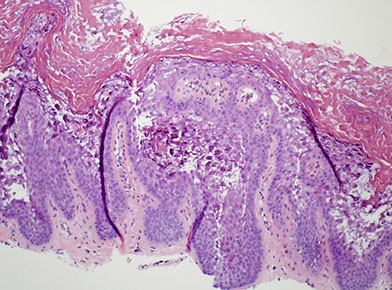
Condyloma acuminatum
Condyloma acuminatum is, by definition, a papillary proliferation with low-grade cytopathic features of HPV infection. The majority are caused by low-risk HPV types 6 and 11. Lesions within this spectrum are designated as LSIL, with the additional optional designation of condyloma in parentheses. Condylomas are common in external anogenital
areas and less frequent in the cervix and vagina. [1]
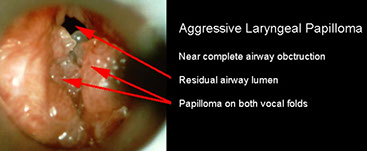
B9, HPV (usually subtypes 6 and 11) caused squamous prolif; usually multifocal
- condyloma latum is caused by syphilis
- women that are pregnant must get a c-section to prevent juvenile-onset recurrent layngeal papillomatosis (which could choke the child)
Micro: blunt arborizing papillae, papillary squames, parakeratosis, koilocytes
- can see some dysplastic changes
- koilocytic atypia = nuclear enlargement, hyperchromasia, cytoplasmic perinuclear halo
Cyto: big nuclei c halos
Tx: topicals, cryosurg, excision
Px: are (usually) not cancerous lesions

Condyloma acuminatum
Condyloma acuminatum - koilocytic atypia


Leukoplakia
White plaques that cause itching and scaling
- may be due to inflammatory or spectrum of malignant disorders (psoriasis, dermatitis, lichen sclerosus, sq cell hyperplasia, VIN, Paget dz, and invasive ca)
Lichen sclerosus

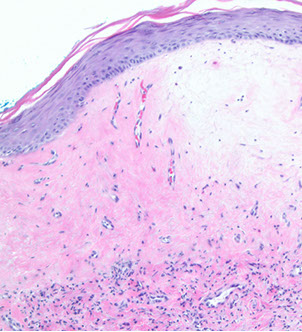
Lichen sclerosus
aka lichen sclerosus et atrophicus
chronic disease with lots of lymphs, usually in post-menopause which itches a lot
- MC in post-menopausal women, may be 2/2 autoimmune dz
Gross: atrophic, thin skin (cigarette paper) with white-red patches
Micro: Marked thinning of epidermis c basal cell degeneration, hyperkeratosis (excessive keratinization), loss of rete pegs, vacuolar interface rxn pattern c dermal sclerosis bwt chronic inflam and epithelium / vessel walls
Tx: best if caught early; topical roids, then oral roids
- should bx to r/o malignancy, may turn to SCC (1/5 get SCC after 4 yrs)
Px: in rare cases assoc c carcinoma, there is p53 overexpression
Squamous cell hyperplasia
aka hyperplastic dystrophy or lichen simplex chronicus
- non-specific rxn to pruritis
- may be present at the borders of malignant lesions
Micro: can have inc mits, but lacks atypia
Squamous cell hyperplasia

Vulvar epithelial (stromal) polyp
Skin tag, similar to other places on body
- just fibrous tissue, which can have myxoid stroma, mits and bizarre stromal cells
Vulvar epithelial stromal polyp

Vulvar squamous papilloma
b9 exophytic prolif covered by non-keratinized sq epithelium which can be single of multiple (as in vulvar papillomatosis)
- unknown etiology
Botryoid rhabdomyosarcoma
aka sarcoma botyroides
- 90% in females <5 yo, 2/3 in 1st 2 yrs
Micro: undifferentiated round or stromal cells are in myoid stroma
- cross striation may be in the cells
- tumor cells crowd around BVs
- cambium layer of Nicholson forms distinct zone
- may involve overlying vaginal epithelium
- may see neoplastic cartilage in older pts with dz higher in the vagina (indicates better px)
Botryoid rhabdomyosarcoma


Rhabdomyoma
Bump in an elderly pt
Rhabdomyoma

Epidermolyic Acanthoma (EA)
B9, asymptomatic, solitary or multiple
- not assoc c HPV or STD
Micro: small, well-circumscribed polypoid with compact hyperkeratosis, acanthosis, hypergranulosis
- keratinocytes inupper epidermis c vacuolated cytoplasm
Px: No inc risk of SCC
Epidermolytic Acanthoma

Extramammary Paget disease of vulva
- aka Vulvar Paget Disease (PD)
Rare, <2% of vulva maligs; classification system based on origin; more often on labia majora, sometimes clitoris
- slowly expanding, sometimes crusting well-defined rash that can be multifocal and have puritic discharge
- dx needs to be done histologically
- vs Paget dz of the nipple, is not usually assoc c underlying cancer and is confined to the epidermis, and can be treated with wide local excision
- is assoc c underlying invasive carcinoma in ~1/3 or less
Micro: pale, foamy cells c microscopic spread usually beyond gross borders of rash
- acanthosis, erosion / ulcers, hyper-/ and parakeratosis in epidermis
- intraepidermal spreading of single/clustered large cells c lots of red to clear cytoplasm, small nucleoli, round nuclei
Cyto: round to columnar kinda big atypical cells that can be single or in groups c lots of clear cytoplasm and vesicular nuclei c nucleoli
IHC: (+) D-PAS, mucicarmine, cytokeratins (CK7, CEA, CAM5.2), GCDFP-15, MUC1, MUC5AC
- negative: S100, MelanA, HMB45, PR, p63, p40, uroplakin III, CK20
- p16 can rarely be strongly positive, which can be a potenital pitfall when VIN is considered in the DDx
- Her2 overexpression has been seen in up to 58% of vulvar PD and has been shown to correlate with presence of invasion, although may predict response to Her2-based targeted therapy [1]
- IHC dependent on source: if secondary to anorectal ca, is CK20+, and CK7 and GCDFP-15
-- secondary to urothelial ca: CK7/20+, GCDFP15 ng-
DDx: morphologic mimics of primary vulvar Paget disease (PD) include pagetoid VIN/ SCC in situ and in situ melanoma
- should consider secondary vulvar involvement of colorectal carcinoma and urinary tract malignancies
- pagetoid VIN and melanoma do not express cytokeratins (CAM5.2, CK7 and CEA) or GCDFP-15
- melanoma will express melanoma markers (which will be negative in primary vulvar PD)
- positive CK20 or CDX2 suggests spread from a colorectal primary malignancy
- Co-expression of CK7/CK20 and uroplakin-III is characteristic of PD secondary to urothelial carcinoma
Tx: Moh's, topical chemo
Px: affected by presence of nodule in lesion, invasion and LN involvement
- staining by p53, cyclin D1, Ki67, and decreased E-cadherin px' significant

Extramammary Paget dz of vulva
A, Vulvar Paget disease. The neoplastic glandular cells in the epidermis stain strongly with cytokeratin 7 (CK7) (B), carcinoembryonic antigen (CEA) (C), and human epidermal growth factor receptor 2 (Her2) (D) (hematoxylin-eosin, original magnification x10 [A]; original magnification x10 [B]; original magnification x20 [C and D]).

Vaginal Intraepithelial Neoplasia (VaIN)
Rare; 40-60% are assoc c HPV
Tx: not amenable to local resection [1]
VaIN 1. The nuclei in the lower one third of the epithelium are enlarged with variable size and increased nuclear-to-cytoplasmic ratios. Cells in the upper layers show changes associated with HPV infection including nuclear size variability, multinucleation or binucleation, and cytoplasmic koilocytic change. Abnormal mitoses and marked nuclear atypia are not present [1]

Dr. Kang LASOP lecture 6/14/22. DEVIL = Differentiated Exophyic vular intraepithelial lesion. VAAD = Vulvar acanthosis with altered differentiaion.
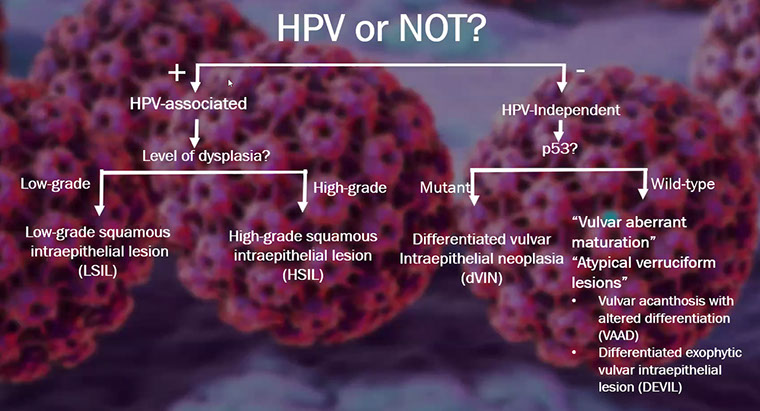
Vulvar Intraepithelial Neoplasia (VIN) and Vulvar Carcinoma
Different subtypes of VIN may lead to different types of carcinoma
- VIN subtypes differentiated, basal, warty
- vs Paget dz of breast which is usually assoc c ca, Paget dz of the vulva assoc c ca in ~25%
Type 1
Basaloid and warty carcinomas assoc c infx c high-risk HPV (in 1/3of cases), usually HPV-16 and Condyloma
- is the less common subtype and occurs at younger ages that smoke cigarettes
- develop from in situ precursor called classic vulvar intraepithelial neoplasia (VIN), usually in women of reproductive age and include lesions previously called Bowen disease or carcinoma
- risk factors for carcinoma are the same as those for cervical carcinoma (young age at first intercourse, multiple partners)
- VIN usually multicentric, usually also have vaginal or cervical HPV
- younger women may have spontaneous regression of VIN lesions, although the risk of transformation to invasive ca is higher in women >45 yo or if immunosuppressed, can turn to basaloid poorly-differentiated carcinoma
Verrucous carcinoma may be assoc c these lesions, presents as big fungating tumor, not much and has a fairly good px (no LN mets) though can be aggressive locally
Tx: excision
basaloid VIN


Verrucous carcinoma
Bowenoid papulosis


.jpg?crc=232845911)
A, Vulva: HSIL (Bowenoid papulosis). the entire extent of the high-grade lesion can be seen, and given the small size and location, Bowenoid papulosis can be included in parentheses in the diagnoses.
Type 2
Differentiated or Simplex subtype of VIN (dVIN) is a unique subtype seen in post-menopausal women presenting as an ill-defined gray-white plaque associated with lichen sclerosus, and more likely than warty to progress to invasive SCC and is high-grade by definition (regardless of extent of maturation)
- may not be recognized if bx too superficial, not assoc c HPV, assoc c cigarette smoking;
- usually a difficult dx to make bc often has overlapping features with b9 hyperplasia, lichen sclerosus and lichen planus
- frequently have p53 mutations
Keratinizing SCC usually in women with lichen sclerosus or sq cell hyperplasia and is not related to HPV
- usually occurs in women around 70 yo
- precursor lesion is differentiated VIN (aka VIN simplex)
Micro: epidermis of dVIN usually thick and hyperkeratotic and/or parakeratotic with elongated and anastamosing rete ridges
- the basal cells show atypical, hyperchromatic nuclei often with inc mits
- upper layers made of enlarged squamous cells with abundant eosinophilic cytoplasm
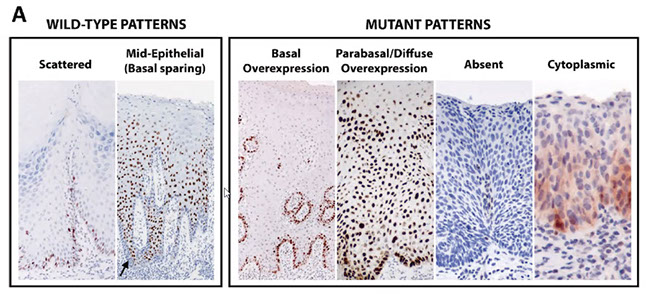
IHC:
p53 IHC patterns in dVIN:
(1) Null pattern;
(2) Strong, uniform nuclear staining in >= 70-80% of basal cells +/- parabasal extension (>1/3 epithelial thickness;
(3) Cytoplasmic positivity
(Tessier-Cloutier B et al Mod Pathol 2020; 33(8): 1595-605)
- Ki67 increased in basal and parabasal cell layers
- CK7+ / CK20-
- negative p16
DDx: p53 overexpression has been reported in lichen sclerosus and other nonneoplastic conditions due to nonmutational upregulation of p53
Tx: surgical, w LN dissection
Px: depends on LN spread (node status)
- lesions <2 cm have 90% 5-yr survival
- much higher rates of vSCC than HSIL

Differentiated VIN

Differentiated VIN - p53

A, Differentiated vulvar intraepithelial neoplasia (dVIN) with marked nuclear atypia and hyperchromasia of the basal cell layer. P53 immunostaining is strongly positive in the lower one-third to two-thirds of the epithelium (B) (hematoxylin-eosin, original magnification x20 [A]; original magnification x20 [B]).
p53 IHC patterns in dVIN: (1) Null pattern; (2) Strong, uniform nuclear staining in >= 70-80% of basal cells +/- parabasal extension (>1/3 epithelial thickness; (3) Cytoplasmic positivity
Differentiated VIN (dVIN) histopathology (Dr. Kang LASOP 6.14.22)


Basaloid dVIN mimicking HSIL (LASOP lecture 6/14/22)

Superficially invasive squamous cell carcinoma (SISCCA)
Vagina [1]
No recommendations have been offered for early invasive squamous carcinoma of the vagina, due to the rarity of primary SCC of the vagina and because insufficient data is available from this site
Vulva [1]
Defined as an AJCC T1a (FIGO 1A) vulvar cancer.
Definition of a T1a vulvar carcinoma:
- Tumor <2 cm in size, confined to the vulva or perineum, AND
- Stromal invasion <1 cm
Note: the depth of invasion is defined as the measurement of the tumor from the epithelial-stromal junction of the adjacent most superficial dermal papilla to the deepest point of invasion
In cases of SISCCA, the following parameters should be included in the pathology report [1]:
- The presence or absence of LVI.
- The presence, number, and size of independent multifocal carcinomas (after excluding the possibility of a single carcinoma).
HPV-related adenocarcinoma of the lower anogenital tract
Micro: histomorphology and cytologic features similar to those of HPV-related endocervical adenocarcinomas (papillary, villiform, villoglandular)
Adenocarcinoma

Angiomyofibroblastoma
B9, Well-circ, small lesions during reproductive age
Tumor cells around thin walled BVs
- have hyper- and hypo-cellular areas, minimal stromal mucin
- mits rare
IHC: (+) muscle markers, cD34, ER/PR
May be on a spectrum with Aggressive angiomyxoma
Angiomyofibroblastoma

(Aggressive) Angiomyxoma
Rare, infiltrates (slowly) locally in reproductive women, can affect some men(???) and has been found in the vagina
Gross: pedunculated vulvar mass (can kinda look like a penis)
Micro: monotonous, uniformly hypocellular, small spindled and stellate fibroblasts w/o atypia, very rare mits (none are atypical)
- myxoid stroma c collagen and thick-walled vessels (hyaline thickening of adventitia)
- can see RBCs extravasated
- may have chondroid metaplasia
IHC: (+) CD23, vimentin, ER/PR, SMA, HMGA2 (sens [+ in 1/2] but not spec, also focal)
- negative: CD117, B-catenin, CKs, S100, EMA, caldesmin, MDM2
Genes: HMGA2 gene at 12q15 (sens but not spec)
- also t(12;21)(q15;q21.1) or t(11;12)(q23;q15)
Tx: wide excision, lifelong FU (has very infiltrative borders)
- chemorads not effective bc slow growing
Px: locally aggressive (1/3 recur locally), but does NOT met


Agressive angiomyxoma (pathoutlines)
Vaginal Adenosis
Women c DES exposure, see metaplastic glandular cells in the vaginal
- anterior 1/3 vag wall
- 1/5 c congenital cervical malformations
- may be a precursor to CCA of the vagina
Vaginal adenosis

Clear cell adenocarcinoma (CCA) of the vagina
Rare (1/10 vag cancers, although 2/3 of CCA occur in the vag) assoc c DES in younger women or no exposure to DES in older women, thus bimodal age distribution (peaks at 22 and 55 yrs)
Micro: cystic, papillary, tubulo-glandular and solid patterns
- can have foci of necrosis
- cell have well-defined membranes, cuboidal to hobnailed, nuclei can be round or irreg
Cyto: good for about 1/2 of cases, can see cells c glycogen vacuoles in clusters, papillae or sheets
EM: looks like CCA of cervix and ovaries
IHC: CK7, CEA, 34BE12, bcl2, vimentin, p53, CA-125, CAM5.2
- negative: CK20 and PR
Tx: surgery for low stage
Px: older pts (second hump, no DES exposure) have worse px, but is generally favorable if low stage, lots mits, and no high grade atypia
- can recur 2-8 yrs after

Clear cell adenocarcinoma of the vagina
Granular cell tumor
May be S100 (+) 2/2 schwannian origin
- may cause pseudoepitheliomatous hyperplasia if forms in the sub-dermis, and can be mistaken for SCC
micro: cells c small dark round nuclei c lots of eosinphilic cytoplasm and eosinophilic granules
- usually c fibrous septae
- malignant feature can occur (high nc, mits (>2/10 hpf), big nucleoli, pleomorphism,
- IHC: (+) S100 (strong and diffuse), PAS, Diastase-resistent (granules),
- px: can met widely and recur after excision
Granular cell tumor

Papillary Hidroadenoma
Sharply circumscribed nodule, usually on labia majora and interlabial folds
- arises from anogenital mammary-like glands along the milk line (are kinda like accessory breasts) in the vulva (esp bwt the labia majora and minora)
- may clinically look like carcinoma bc can ulcerate
Micro: identical to intraductal papilloma of the breast c papillary projections covered by 2 layers of cells (myoepithalial cells and columnar secretory cells
- the crowded glands may raise concern for carcinoma, but this is ruled out by a 2-cell layer
IHC: (+) EMA, Calponin, (stains both cell layers)
Papillary hidroadenoma

Melanoma
2nd MCC malignant neoplasm of vulva
- may look like Paget dz
References
1. Darragh et al. CAP-ASCCP LAST Project. Arch Pathol Lab Med; vol 136, Oct 2012
