Urinary Cytology
General
Normal urothelium
Transitional cells
Columnar cells
Ureteral cells
Squamous epithelial cells
Prostatic cells
Seminal cesicle cells
Histiocytes
Melamed-Wolinska bodies
Hematocyturia
Bladder / lower UTI
Herpes
Cytomegalovirus
Polyomavirus
Trichomonas
Schistosoma haematobium
Mycotic infx
Eosinophiluria
Lymphocyturia
Malacoplakia
Urinary Calculi
-
Non-pathogenic
- Calcium sulfate
- Calcium carbonate
- Uric acid
- Triple phosphate
- Calcium oxalate
-
Pathogenic crystals
- Cholesterol
- Cystine
- Trypsine
- Leucine
- Sulfonamides
Renal casts
- Hyaline casts
- Granular casts
- Renal tubular epithelial casts
- Leukocyte casts
Rejection of renal transplant
Ileal conduits
Intravenous pyelogram
Reactive Cells
Dysplastic cells
Carcinoma cells
Carcinoma-in-situ
Papilloma
Squamous cell carcinoma (epidermoid)
Adenocarcinoma
Conventional RCC
PUNLMP
Urothelial ca
- low-grade urothelial ca
- high-grade urothelial ca
Myelolipoma of adrenal gland
Renal Cytology
Urinary Cytology
General
Urine cytology indicated c hematuria, pts at high risk for urologic malig (aniline dye exposure), or the following of urologic malig
- 1st pee of morning avoided bc has been sittin there all night and can cause changes in cells
- for similar reasons, bladder washing may be better than catheterized urine
- upper urinary tract brushing can have high NC, mimicking malig cells; stones can cause similar changes
No fixation needed in cells less than 12 hours old; should be put in fridge if 12-24 hrs old; >24 hrs requires ethanol fixation
Degenerated cells common, and specimens from women often consist almost entirely of squamous cells
Urine cytology is only moderately sensitive at best; though is usually very specific (few false-positives) - though these may occur in pts c stones, post-chemo, or 2/2 polyomavirus
- FISH studies are more sensitive but less specific
Normal Urothelium
Urothelium lined by 3-7 layers of urothelial (transitional) cells, with umbrella cells at surface containing more cytoplasm (low NC) than deeper cells, and can have 2+ nuclei and the size can be highly variable
- usually single cells (rarely in groups); may be found in groups in washings and brushings
- Melamed-Wolinska bodies: red/green cytoplasmic inclusions in degenerated transitional cells that look like macros seen in 1/2 of specimens
Transitional cells
Can come from anywhere from the renal pelvis to the bladder, but mostly the bladder; variable size c transparent basophilic cytoplasm and variably-sized vacuoles (from degeneration)
- central nuclei c finely dispersed chromatin and small nucleoli; multinucleation common; may be single or in small clusters
- deeper transitional cells can have 2+ nuclei
Columnar cells
uncommon; come from the glands in the urinary tract and are single or in small clusters appearing as papillary fronds when coming from a catheter
- can be ciliated and normally have a single mucinous cytoplasmic vacuole
- nuclear chromatin finely granular and small centrally located nuclei are common
Ureteral cells
seen in ureteral catheterization or washing specimens but can be voided in urine
- lots of polymorphism, usually binucleated
Squamous epithelial cells
Intermediate or superficial cells seen in normal urine samples, usually in females; may come from trigone
- Look like vaginal squames and also can show cyclic changes
- may come from distal urethra in males
Prostatic cells
Seldom exfoliated but can be seen after prostatic massage
- cuboidal to columnar and can look round in urine c a round central nucleus that occupies <1/2 of total cell
Seminal vesicle cells
Rarely seen in normal urine samples, except after prostatic massage. [2]
- larger and more irregular than prostatic cells and have golden-orange intracytoplasmic pigmented granules representing lipofuscin (clue that benign)
Histiocytes
Single cells or loose clusters c fomy cytoplasm and eccentric bean-shaped nucleus
- mononucleated but can be multinucleated
Melamed-Wolinska bodies
Epithelial / transitional cells c eosinophilic to green cytoplasmic inclusions
no known significance, but may be a clue that malignant cells originate from urothelial tract [2]
- may be the result of degeneration as the nuclei are often degenerated
- has red round cytoplasmic inclusions
Hematocytouria
RBCs in varying numbers can be 2/2 renal dz, calculi, tumors, acute infx, infarction, renal vein thrombus, hydronephrosis, polycystic kidney dz, or acute / chronic infx of lower urinary tract
- hematuria assoc c malig in only up to 1/10 cases
Bladder / lower UTI
Can see neutrophils engulfed in the cytoplasm of urothelial cells
- reactive urothelial cells c enlargement r pyknosis of the nucleus and vacuolated or ill-defined cytoplasm
Herpes
May be picked up in urine or rarely involve urothelial cells
- esp seen in immunosuppressed
- have same old "ground-glass" appearance c chromatin condensation at nuclear borders
Cytomegalovirus
Can affect urothelial or renal tubular cells
- large round basophilic nuclear inclusion while herpes inclusions are eosinophilic
- can have cytoplasmic inclusions, whereas herpes inclusions are nuclear
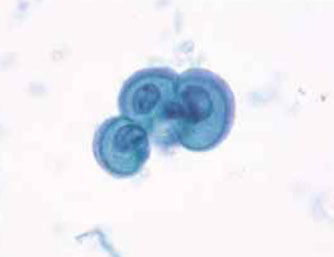
Polyomavirus
Polyomaviruses (JC and BK viruses) commonly affect urothelial cells of both healthy and immunocompromised individuals. Characteristic viral cytopathic changes are seen in 4% of urine samples. The infection usually has no clinical significance, except in immunocompromised (transplant) patients
- nickname is "decoy cells"
Cyto: Infected urothelial cells have large eccentrically placed nuclei with basophilic nuclear inclusions that completely replace the nucleus and appear glassy, opaque or cloudy.
- because of increased nuclear size and hyperchromasia, these cells are sometimes confused with malignant cells – hence their pseudonym “decoy cells”. However unlike most malignant cells , decoy cells have perfectly smooth and round nuclei.
IHC: (+) SV 40
Trichomonas
Has same morphologic patter as in vaginal smears
Schistosoma haematobium
Develops around the egs; mucosa can undergo squamous metaplasia
Mycotic infx
Found in elderly or diabetic pts or those tx'd c chemo
- cytology shows leukocytes, debris, hyphae and spores of fungi
- MCC is candida or aspergillus
Eosinophiluria
Assoc c chronic inflam, drug hypersensitivity and parasitic infx
Lymphocyturia
Indicates a chronic inflam process
- often seen in large numbers in acute renal allograft rejection, lupus nephritis and viral infx
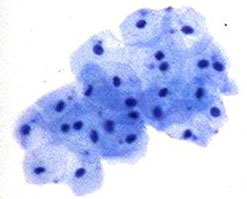
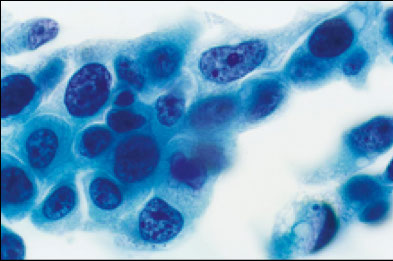
Malakoplakia
Rare chronic inflammatory (granulomatous) lesion in middle-aged women on the bladder wall or from upper urinary tract
- appears as a soft yellow plaque
- made of iron and calcium, are due to incomplete intracellular digestion of engulfed microorganisms by macrophages causing accumulation of intracellular materials
Micro: large amts of plump histiocytes, which can be multinucleated
- may have chronic inflam infiltrate
- Michaelis-Gutmann bodies (laminated calospheres, usually basophilic, w/in cytoplasm of histiocytes or extracellular)
Urinary calculi
Enlarged nuclei c coarse chromatin, condensation of chromatin at nuclear border and sometimes multinucleation
- difficult to differentiation from malignant cells, but have lesser degree of nuclear pleomorphism and no loss of nuclear polarity
- prolonged lithiasis can produce squamous metaplasia
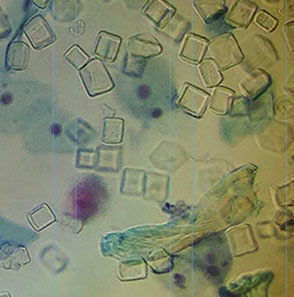
Nonpathogenic crystals
Calcium sulfate - seen in acidic urine
- small transparent needles, singly or in clusters
Caclium carbonate - seen in alkaline urine
- very small, round or dumbbell shaped
Uric acid - assoc c elevated serum uric acid
- semitransparent yellow to brown, hexagonal, star-like or diamond shaped or even butterfly-shaped
Triple phosphate - in alkaline urine
- elongated, transparent rectangular or diamond-shaped (coffin-shaped)
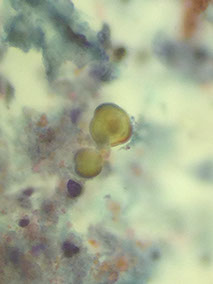
Pathogenic crystals
Cholesterol - indicative of renal disease
- transparent with irregular edges that look like fragments of broken glass
Cysteine - assoc c a cysteine calculus and some metabolic disorders
- transparent, refractile hexagonal plates that are variably-sized
Tyrosine - usually is diagnostic of advanced liver disease
- fine needles arranged in sheaves or clumps, and are usually yellow
Leucine - also can be indicative of severe liver damage
- yellowish-brown, oily globules with concentric rings and radial striations
Sulfonamides - see following the administration of drugs
- yellow-brown asymmetrical triangular sheaves or round forms with radial striations
Renal casts
Form when proteins precipitate and conglomerate in the tubular lamina
- when they appear in the urine they reflect the shapes and diameters of the renal tubular lumina of origin
- may be strait or convoluted, although typical casts have parallel sides and round blunted ends
-- casts with long, thin tapering tails have no significance
Fatty casts - have lipid vacuoles, seen c nephrotic syndrome
Hyaline casts - basic protein considered physiologic 2/2 decreased urine flow or high protein concentration
- semisolid, transparent elements staining light blue
Granular casts - represent breakdown of products of renal epithelial lining and may be assoc c renal parenchymal disease
- vary in size and composition and have fine or coarse granular inclusions, staining gray-orange or bluish-green
RBC casts - assoc c glomerular dz
Renal tubular epithelial casts - made by desquamation of renal lining cells
- can occur in renal parenchymal dz or damaged or renal allograft rejection
- contains 2 parallel rows of cells; epithelial cells must be distinguished from neutros
Leukocyte casts - MC in pyelonephritis
- have the morphologic detailing of leukocytes, not always easy to distinguish
Ileal conduits
Created when a cystectomy is performed
- urine from ileal conduits can show degenerated intestine epithelial cells and urinary tract cells and possible recurrent urinary tract tumor cells
- usually have red cytoplasmic inclusions
Intravenous pyelogram
Makes small sheets of atypical cells
- globules of dye staining gray can be engulfed by histiocytes
- giant histiocytes can be seen
Rejection of Renal Transplant
5 of the following 7 criteria indicate rejection:
- nuclear changes
- casts
- RBCs
- "dirty" background
- mixed cell cluster
- lymphocytes
- renal tubular cells (**most important criterion! esp if degenerating [smaller, shed singly, eccentric pyknotic nucleus])
Reactive Cells
Central (non-eccentric) nucleus; N/C normal to slight inc
- borders are smooth c fine evenly distributed chromatin; large nucleoli present; vacuolated cytoplasm
Dysplastic cells
Slightly inc NC; central to eccentric nucleus, c notches, fine and hyperchromatic chromatin, evenly distributed chomatin; absent nucleoli, homogenous cytoplasm
Carcinoma cells
Inc NC; eccentric nucleus c pleomorphic irregular borders coarse and hyperchromatic chromatin, unevenly distributed; absent nucleoli unless is a high grade tumor; homogenous cytoplasm
Carcinoma-in situ (CIS)
A non-papillary neoplasm where the transitional epithelium is completely replaced by anaplastic cells but does not invade the underlying CT
Papilloma
Gross: Neoplasm that grows into the lumen of the bladder and is made of transitional epithelium
- rare and occur mostly in younger pts [2]
The punchline after seeing papillary clusters:
- the presence of papillary clusters may be 2/2 instrumentation effect, a papillary urothelial neoplasm or renal calculi
Micro: central core of loose connective tissue with a a covering of transitional epithelium
- individual cells look normal, don't invade or met
- can be suggestive on cytology but cannot be dx'd
Squamous cell carcinoma (epidermoid)
Looks like squamous cell carcinoma seen in other organs, like cervix or lung
- usually is derived from papillary tumors, vesicular leukoplakia that can accompany calculi, or following schistosomiasis
- see keratinization and pearl formation and intercellular bridging
Adenocarcinoma
Made of glandular epithelium, and is usually well-differentiated and often partially or completely mucus-producing
Normal urothelium - umbrella cells
Normal urothelial cells c single round nucleus (ThinPrep)

Deep transitional cells, similar to superficial cells but with denser blue cytoplasm
Columnar cells

Melamed-Wolinska body


Polyomavirus
Malakoplakia

uric acid crystals

triple phosphate
Leucine

sulfazidine crystals

Cystine
RBC cast


WBC cast
Epithelial cast

Granular cast
Ileal conduit urine: cellular specimen c degenerated single cells and few glandular cells in dirty background


Reactive cells
Dysplastic cells


CIS: Markely atypical cells c hyperchromatic angulated nuclei, coarse chromatin, irreg nuclear contours, and occasional prominent nucleoli. NC ratio is high and cytoplasm is dense
Squamous cell ca
Adenocarcinoma


PUNLMP
Papillary urothelial neoplasm of low malignant potenital (PUNLMP)
- used to be called transitional cell carcinoma, grade 1
- not really considered carcinoma, rarely (10%) progress to carcinoma [2]
- defined as a papillary lesion c minimal or absent atypia but inc cellular prolif greater than the thickness of normal urothelium
Micro: looks like slightly atypical papillomas or not atypical, but occurring in older pts and with greater cellular thickness
Urothelial Ca.
Etiology: Smoking and exposure to industrial compounds
- MC neoplasm of the urinary tract
- can be papillary or non-papillary
Papillary has fine CT core with thin-walled vessels and a covering of 4-6 layers of transitional epithelium
- papillary fronds are seen covered by epithelium c inc cellularity, loss of polarity, cellular pleomorphism, nuclear hyperchromasia and mitotic activity and is larger than a papilloma
Non-papillary is an infiltrative transitional cell carcinoma that looks flat and plaque-like c or without ulceration
- there is dec adhesiveness of cells and more cells are exfoliated
UroVysion
FISH test to look for amplification of chromosomes 3, 7, and 17 or deletion of chromosome 9 (at 9p21)
*** prime numbers!!! (except 9) ***
- 3 is red, 7 green, 9 gold, 17 aqua
Low-Grade Urothelial cell Ca.
Criteria [2]:
Cytoplasmic homogeneity, inc NC, irregular nuclear mem.;
- absent nucleoli
Papillary fragments c fibrovascular cores is diagnostic (though rarely seen)
- also have more irregular edges in cell clusters and sheds off single cells (more than in benign groups)
- low sensitivity but higher specificity; may not even be reportable bc rarely progress, thus may be more accurate to state in report "negative for high-grade malignancy"
Tx: intravesical bacillus Calmette-Guerin (bCG) sometimes given to prevent recurrence of superficial urothelial carcinomas and can cause a granulomatous response in the wall of the urinary bladder (get loose aggregates of epithelioid histiocytes c MNGCs [Langerhans type])
High-Grade Urothelial cell Ca.
May refer to a tumor that is invasive or not
Criteria [2]:
High N:C; hyperchromatic nuclei; coarsely granular chromatin; irregular nuclear outline; large nucleoli (occasionally)
- cells can have Melamed-Wolinska bodies and background can be necrotic
- has much higher sensitivities and specificities than low-grade ca
Other Criteria for HGUC [3]:
• High N/C ratio. Malignant cells should have an
N/C ratio of 0.7 or greater, meaning that the
nucleus occupies at least 70% of the cytoplasm.
• Moderate-to-severe hyperchromasia. Practically,
the amount of hyperchromasia should be sufficient
to distinguish clearly the amount of chromasia
from that of bystander benign urothelial
cells.
• Markedly irregular nuclear borders.
• Coarse, clumpy chromatin.
The criteria for the SHGUC category are:
• High N/C ratio. Atypical cells should have an N/
C ratio of at least 0.5.
• Moderate-to-severe hyperchromasia.
Additionally, one of the following two features
must be present:
• Markedly, irregular nuclear borders.
• Coarse, clumpy chromatin.
The criteria for the Atypical Urothelial Cells (AUC) category are:
• High N/C ratio. Atypical cells should have an N/
C ratio of at least 0.5.
And one of the following:
• Hyperchromasia. The hyperchromasia may not
be as pronounced as in HGUC or Suspicious for
HGUC, but still distinct from what is seen in the
surrounding benign urothelial cells.
• Irregular nuclear borders.
• Coarse, clumpy chromatin.
Because the AUC category implies
"Coy cells" - cells in a high-grade malignancy that are rare, small hyperchromatic and with highly irregular nuc mems

PUNLMP. Papillary clusters of urothelial cells c homogeneous cytoplasm, nuclear enlargement, and eccentric nuclei. Nuclei should have smooth nuclear contours and slightly granular cytoplasm and occasional nuclei



High-grade urothelial cell ca's (up and left)

Low-grade urothelial ca: Clusters of urothelial cells c enlarged nuclei, irregular nuclear membranes, slightly inc NC ratio and homogeneous cytoplasm

HG papillary urothelial CA: clusters of marked atypia c pleomorphic nuclei, coarse chromatin and prominent nucleoli. Cytoplasm can range from dense to vacuolated. Irreg nuclear contours and irreg coarse chromatin, nucleoli are frequently present

(b) Example of a cell meeting the criteria for the Suspicious for High-Grade Urothelial Carcinoma category; this cell has an N/C ratio just below 0.7 and demonstrates severe hyperchromasia, clumpy chromatin and markedly irregular nuclear borders. If this cell had an N/C ratio of above 0.7, it would meet the cytomorphological (but not quantitative) criteria
for the High-Grade Urothelial Carcinoma category.
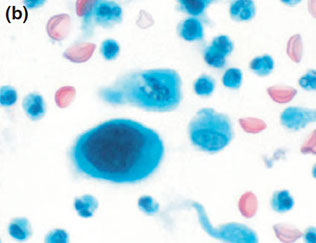
a) Example of a cell meeting the criteria for the Atypia Urothelial Cells category; this cell has an N/C ratio of approximately 0.5 and demonstrates coarse chromatin, although only mild hyperchromasia and only mildly irregular nuclear borders.

(c) Example of a cell meeting the cytomorphological criteria for the High-Grade Urothelial Carcinoma category; this cell has an N/C ratio of above 0.7, along with coarse chromatin, severe hyperchromasia
and markedly irregular nuclear borders.
Myelolipoma of the adrenal gland
Composed of adipose tissue and benign hematopoietic elements (nRBC, megs, granulocytes and their precursors)


Myelolipoma of adenal gland
Renal Cytology
Overview
vimentin good to differentiate oncocytoma and chromophobe RCC from other tumors, CAIX is positive mostly in CCRCC ,while CK7 is + in chromophobe RCC and papillary RCC type I, racemase is + in papillary RCCs, and TFE3/TFEB fairly specific for translocation RCC
- cytogenetics can be done on cytology specimens
Angiomyolipoma
May be part of tuberous sclerosis complex, F>M
- fat poor variant is challenging on imaging, which is why it gets bx'd
IHC: (+) SNA, HMB45, ER/PR
- neg: PAX8, CK7
Genes: TSC1 (cr9) and TSC2 (cr16)
Chromophobe RCC, Oncocyic variant
Rarely multifocal, has overlapping variant with renal oncocytoma
- PAX8+, vimentin neg, CK7+, CD117+, E-cadherin+, neg S100
Genes: lots of chromosomal losses
Px: excellent, except sarcomatoid variant
Papillary RCC, Type I (basophilic)
Small nuclei c scant basophilic or amphophilic cytoplasm (low-grade nuclei); is usually cystic and necrotic, thus non-enhancing on imaging)
IHC: (+) vimentin, CK7, racemase,
- neg: CAIX, WT1
Genes: trisomy 7 and 17, loss of Y
Papillary RCC, Type 2 (eosinophilic variant)
Usually multifocal, hemorrhagic and necrotic
-Nuclei c prominent nucleoli (high grade nuceli) and abundant eosinophilic cytoplasm
IHC: PAX8+, vimentin+, CK7-/+, CD117 neg, E-cadherin neg, racemase+, CAIX-/+, TFE3 neg
genes: cr 7 trisomy/tetrasomy, cr 12//16/17/20 trisomy or loss of Y
Clear cell RCC ("granular variant")
can be multifocal and part of vHL
- granular var is not a special type
- PAX8+, vimentin+, Ck7-, CD117 neg, e-cadherin neg, racemase neg, CAIX+ (specific)
genes: partial cr3 loss
Mucinous tumor and Spindle Cell RCC
F>M (4:1), morphology and IHC similar to papillary RCC type I
IHC: (+) PAX8, vimentin, CK&, Racemase
- neg: CAIX
genes: numerous losses and gains
Px: good, except sarcomatoid type
Oncocytoma
Part of Birt-Hogg-Dube syndrome, usually seen in older pts
- central scar present on radiology
- 1 of 2 RCCs that are vimentin neg, also PAX8+, E-cadherin+, CD117+, CK7 neg, S100+
Translocation RCC
First described in peds, but is up to 1/50 adult RCCs
- part of the MiTF tumor family (TFE3, TFEB)
IHC: (+)PAX8, vimentin, CAIX, racemase, TFE3/TFEB,
- neg; CK7, HBM45/melanA (-/+)
Px: better in peds
Benign Glomerulus

Conventional RCC
Low power demonstrates large cohesive monolayer sheets of vacuolated cells
Clean background or sometimes bloody
Abundant wispy cytoplasm with ill-defined edges
Large round eccentrically placed nucleus
Nucleoli vary depending on the Furhman grade



Conventional RCC
References
1. Notes, the U
2. Cibus. Cytology. Next to new ed. Ch 3. Bladder and Urine washings
3, VandenBussche CJ. A review of the Paris system for reporting urinary cytology.
