Thyroid Cytology

Thyroid cytology basics
Molecular testing
Bethesda categories
Tracheal contamination
Lymphocytic thyroiditis
Benign nodular goiter
Chronic lymphocytic-Hashimoto Thyroiditis (HT)
Subacute (de Quervain) Thyroiditis
Reidel disease
Follicular Neoplasm
Follicular Neoplasm, Hurthle cell type
Poorly differentiated thyroid Carcinoma (PDTC)
Anaplastic (Undifferentiated) Carcinoma
Medullary Carcinoma
Papillary Thyroid Carcinoma (PTC)
Metastatic carcinoma

Thyroid cyology basics
Up to 1/20 adults have a thyroid nodule, less than 1/20 of those are malignant
- 1/20 nodules are "hot" and don't need FNA, which is determined by getting TSH levels; if TSH is high or normal FNA can be done, if TSH is low then radionucleotide scan can be done to confirm nodule is hot (hyperproducing thyroid hormone) and doesn't need an FNA
- nodules <1 cm not FNA'd unless they have suspicious characteristics (microcalcifications)
- penetrating into larynx and esophagus causes the pt to cough, and ciliated cells can be seen on FNA
Non-dignostic / Insufficient for Diagnosis (IFD) - need at least 6 groups of 10 cells per group to be called a diagnostic specimen; IFD risk of malignancy is up to 4% and thus FNA should be repeated (up to 9/10 re-FNA'd lesions become diagnostic)
- if a diagnosis is given or if there is atypia, then the specimen is not IFD (logically)
- too much blood or overly thick smears can render a smear IFD
Cyst Fluid Only (CFO) - reported if specimen has only macrophages
- person doing US must then determine if lesion looked benign (entirely cystic) or if it had malignant features, and the lesion is then treated so (CFO's are malignant in 4%)
7/10 FNA'd nodules are benign (multinodular goiter and follicular adenoma); but <1% are false-negatives and thus still require FU
- most benign lesions are paucicellular and have lots of colloid
1/10 nodules are suspicous; can be suspcious for: Hurthle cell neoplasm, follicular neoplasm or malignancy (usually papillary ca)
1/20 are malignant, and is usually a papillary ca; these specimens are usually hypercellular c architectural atypia
Hurthle cells - metaplastic follicular cells c lots of mitochondria
Molecular testing
- even though tests are expensive, costs may level out considering the surgeries that are not performed
BRAF - very specific (100%), but not sens, provides additional px info
ThyGenX - 7 gene panel, high spec (up to 100%), lower sens, positive results RULES IN cancer, though negative result does not rule out cancer c high certainty, with the specific mutation providing px info
Thyroseq v.2 (CBLPath)- Next gen DNA sequencing-based test for numerous genetic alterations assoc c cancer (and one c benignity), high sens and spec, potentially function BOTH as rule out and rule in test; although only 2 tests done which were both done by the producers of the test; the specific mutation can provide px info
- $3200 list price, CPT code 81479 (Tier 2 molecular pathology procedure)
Afirma (Veracyte) - Gene expression classifier - mRNA expression (25 genes to ID mets, parathyroid, MTC, Hurthle cells, and 142 gene for b9 vs malig), designed to maximize sens, neg test RULES OUT malig, can avoid surgery in AUS and SFM that are negative; has lower spec, suspicous should be treated as non-informative, esp for Hurthle cell lesions; requires cytology specimens be read at partner cytology lab ( c some exception); medicare rate: $3220 (no copay); optional BRAF = $180
Negative predictive value:
– AUS/FLUS= 95%
– FN/SFN= 94%
ThyraMIR - MicroRNA-based GEC, designed as reflex test for ThyGenX-neg nodules; combined sens 89%, combined sens 85%, attempt to add ability to RULE OUT to ThyGenX
All the above based on current classification of NFVPTC as malignant, reclassification will ldec spec, PPV of all tests, tests should be redesigned, and test performance should be repeated
5-10%
or molecular
now 45-60% c NIFTP
6-18% c NIFTP
94=96% c NIFTP
/molecular

Follicular cells


Hurthle cells
Colloid - can only trust the thick colloid, the thin colloid can actually be plasma

Macrophages
Oncocytic cells

Sk -muscle
Cyst Lining cells
• Elongated shape
• Distinct cell borders
• Abundant cytoplasm
• Most are easily recognized as benign
• But sometimes the degree of atypia is
sufficient for a dx of AUS/FLUS
Cyst Lining Cells

H&E
Thyroglobulin
Cyst Lining Cells

Cyst Lining Cells

Cyst Lining Cells

Bethesda Categories
I. Nondiagnostic or Unsatisfactory
Cyst fluid only
- Virtually acellular specimen
- Other (obscuring blood, clotting artifact etc.)
*Adequacy of Thyroid FNA’s require at the minimum 6 follicles containing at least 10 well visualized follicular cells
Exceptions:
Significant cytologic atypia, inflammatory nodules , or a nodule with abundant colloid

Cyst fluid only, Cat I
II. Benign
up to 70% of all thyroid FNAs
Benign follicular nodule MC benign pattern: an adequately cellular specimen composed of varying proportions of colloid and benign follicular cells arranged as macrofollicles and macrofollicle fragments. If resected, virtually all benign follicular nodules turn out to be nodules of a multinodular goiter or follicular adenomas. This distinction cannot be made by FNA and is of no consequence to the patient
Characteristics: usually multiple nodules (but can be solitary); Low to Moderate Cellularity; Multiple Cell Types; Honeycomb Maintained; Variable follicle size; Degeneration/Regeneration Common; Abundant colloid
Consistent with benign follicular nodule (includes adenomatoid nodule, colloid nodule etc.)
- Includes lymphocytic (Hashimoto’s) thyroiditis in the proper clinical context
Consistent with granulomatous (subacute) thyroiditis
Lymphocytic thyroiditis
Encompasses a variety of conditions, including chronic lymphocytic thyroiditis (Graves disease), subacute lymphocytic throiditis (postpartum and silent thyroiditis(, and focal lymphocytic thyroiditis
- chronic lymphocytic thyroiditis is the MC of these
Chronic Lymphocytic Throiditis (Graves dz)
MCC hyperthyroidism; Autoimmune dz c overactive thyroid gland; usually dx'd clinically
- pt presents c diffuse goiter, though palpable nodules can occur
- Cytologic features may overlap other diffusely growing goiters such as Hashimoto’s thyroiditis, granulomatous thyroiditis, diffusely growing cancers
Micro (FNA): High cellularity; Watery colloid; Flame cells ; Hurthle cells; Inflammation; Granulomas
Granulomatous thyroiditis (subacute, de Quervain)
Multinucleated Giant Cells; Epithelioid Histiocytes; Variable inflammation; Scant degenerate follicular cells
Tx: Clinical follow up (risk of malignancy <1%)
II. Benign, hyperplastic nodule

Granulomatous thyroiditis
Lymphocytic (Hashimoto) thyroiditis

III. AUS / FLUS
1-22% of all thyroid FNAs; Atypia of undeternined significance / follicular lesion of undetermined significance, should limit use to 10% of thyroid FNAs
- 6-18% risk of malignancy now considering NIFTP
May subgroup category III in the report if there is any atypia or not (no difference now in tx, but may be useful for studies)
Qualifiers (do not affect management, for internal use
Cytologic atypia
Architectural atypia
Cytologic and architectural atypia
Hürthle cell AUS/FLUS
Atypia, NOS
Atypical lymphoid cells
- FNA is more of a screenng (not diagnostic) for follicular carcinoma (and is the 2nd MCC thyroid ca)
- follicular ca is more aggressive than papillary ca, and mets to lungs and bones
- many lesions that are suspicious for follicular ca turn out to be malignant, the majority of which turn out to be follicular variant of papillary ca, and some as follicular ca
- some cases suspicious for follicular neoplasm turn out to be adenomatoid nodules of MNG
Risk of Malignancy 6-18% now bc non-invasive follicular variant of papillary thyroid CA (NIFTP) no longer considered malignant (used to be 10-30%,)
Macrofollicle does not necessarily mean a large follicle, but more evenly spaced
Microfollicle is crowding, showing a loss of growth control, which is the hallmark of neoplasia
Tx: Repeat FNA and/or molecular testing
- may need to do a completion thyroidectomy bc if found to be malignant, remnant thyroid obscures further Iodine-131 studies (used to detect recurrence / mets)
Molecular testing:
1) Afirma (Veracyte) Gene expression classifier (mRNA-based) that finds the molecular signature of b9 thyeoid nodule
2) ThyroSeq v2 (CBLPath) - Next gen DNA sequencing for pt mutations and gene fusions in known thyroid cancer genes

III. Hurthle cells
III. Hurthle cells

III. Atypia of Undetermined Significance (AUS)

Macrofollicle

Microfollicles
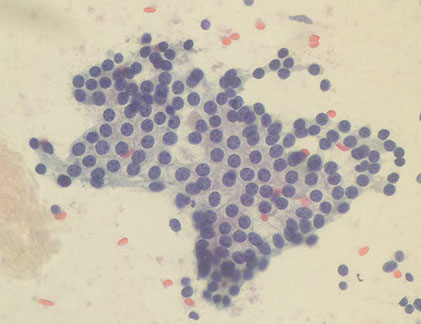
IV. Follicular neoplasm / Suspicious for follicular neoplasm
Includes Follicular Neoplasms and Follicular Nodules
- Cellular Aspirate Comprised of Follicular Cells
- Significant Cell Crowding and/or Microfollicle Formation
- 15-30% of cases dx'd in this category turn out to actually not be neoplasms
Includes Benign follicular nodules, follicular adenoma, follicular carcinoma, Follicular Neoplasm/Hurthle Cell Type, follicular variant of papillary ca
- Excludes Cases with Nuclear Features of Papillary Carcinoma
Usually solitary nodules, High Cellularity / Scant Colloid, Microfollicular Pattern and/or trabeculae; large crowded follicular cells
Nuclei: Round +/- enlargement, Nuclear membrane is smooth to irregular, Chromatin is granular, variably hyperchromatic, Nucleoli usually inconspicuous / absent (except in cancer), Increased n/c ratios
DDx: B9 follicular nodule, PTC, RCC mets, parathyroid ca
Tx: lobe with nodule gets excised (lobectomy)
Suspicious for Follicular Neoplasm, or Follicular neoplasm
- specify if Hurthle cell type
Up to 1/25 of thyroid ca's, similar to other follicular ca's, dx is dependent on capsular or vascular invasion
- 10-40% risk of malignancy considering NIFTP not an overt malignancy
Micro: Follicular-patterned cases c mild nuclear
changes (inc nuclear size, nuclear contour irregularity, and/or chromatin clearing) can be classified as FN/SFN of true papillae and intranuclear pseudoinclusions absent;
- note that some nuclear features raise the possibility of a FV of PTC or NIFTP can be included
- pure Hurthle cell population in follicular, trabeculae or solid growth patterns, which are usually not cohesive, have a prominent nucleolus, granular cytoplasm and pseudopsammoma bodies
- colloid can look more basophilic
Pitfall: Must dx as B9 if there is a MIXTURE of Hurthle cells and normal follicular cells (image)
- will only call AUS/FLUS or Suspicious for Hurthle cell neoplasm if there is a single population of Hurthle cells
DDx: Hashimoto's (hyperplastic nodule), MNG, macrophages, PTC, RCC mets, medullary ca, parathyroid, granular cell tumor
- histopathologic follow-up of cases diagnosed as suspicous for a follicular neoplasm includes follicular adenoma, follicular carcinoma, and follicular variant of papillary thyroid carcinoma, including its recently described indolent counterpart NIFTP
Genes: Hurthle cell neoplasms NEVER have PAX8-PPAR rearrangement (seen in 26-53% of follicular ca)
Tx: lobe with nodule gets excised (lobectomy) or molecular testing
IV. Follicular Neoplasm, Hurthle cell type

Suspicious for a Follicular Neoplasm


Should dx as BENIGN if there is a mix of Hurthle cells and B9 follicular cells, only dx as AUS/FLUS if there is a monomorphic population of Hurthle cells

IV. Follicular neoplasm. Cellular aspirate of follicular cells with a predominantly microfollicular architecture, few single cells and no colloid
V. Suspicious for Malignancy
Specimen contains features for malignancy, but the findings are not sufficient for a conclusive diagnosis.
- Specimens suspicious for a Follicular or Hurthle Cell Neoplasm are excluded from this category.
- morphologic changes are of such a degree that a malignancy is considered more likely than not
- Risk of Malignancy: 45-60% now that NIFTP no longer considered an overt malignancy
Tx: total thyroidectomy or lobectomy
- exception: mets
Suspicious for malignancy

VI. Malignant
Includes: Papillary Carcinoma; Follicular Carcinoma;
Medullary Carcinoma; Poorly Differentiated Carcinoma; Anaplastic/Undifferentiated Carcinoma
(carcinomas discussed below)
- To avoid false-positives due to NIFTP, limit use to cases with features of classical PTC (true papillae, psammoma bodies, nuclear pseudoinclusions).
- exception again: mets
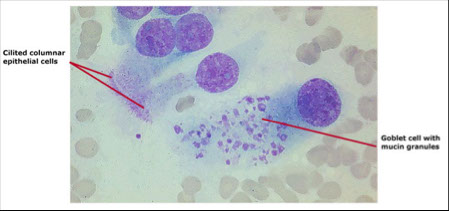
Tracheal contamination
-Foamy cells or mucoid fluid
-Respiratory (ciliated columnar cells) or squamous epithelial cells

Benign nodular goiter
- encompasses Multinodular Goiter (MNG) and follicular adenoma (macrofollicular type)
MNG is MCC endocrine disorder worldwide and is causes by dec iodine consumption (US prevalence around 1/20); are grossly unencapsulated
- TSH inc 2/2 dec thyroid hormone synth; this inc in TSH causes hyperplasia of the follicular cells which causes a somatic genetic mutation causing a clonal proliferation of follicular cells and thus a nodule forms
Follicular adenoma is a solitary enlarged nodule which is well-encapsulated (does NOT invade capsule) - in order to definitively tell whether there is capsular invasion must see it on a tissue section
Micro: macrofollicles in cohesive sheets and spheres c up to moderate cellularity of uniform cells c coarse, dark chromatin
- background includes watery colloid, Hurthle cells, macros and cyst lining cells
- cyst lining cells may appear ugly and degenerative; and Hurtle cells can be metaplastic and ugly as well
Tx: surgery (for younger pts and larger goiters), radioactive iodine, T4 admin (decreases TSH)
- must FU for 3-5 years to ensure is b9
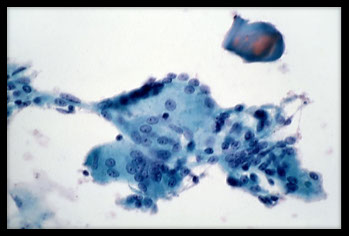
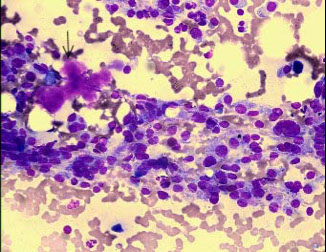
Chronic lymphocytic (Hashimoto) Thyroiditis (HT)
Almost exclusively in perimenopausal women
- autoimmune dz (antithyroid peroxidase, antithyroglobulin abs, and antimicrosomal antibodies) where follicles destroyed by lymphocytes, causing pt to become hypothyroid
- FNA not necessary (unless suspect carcinoma)
- aka lymphocytic thyroiditis c oxyphilia bc has combo of oncocytic (Hurthle) cells and lymphs
Imaging: diffusely heterogenous gland that is hypogenic compared to normal thyroid on US
Micro: lots of lymphs c small atrohpic follicle centers; Hurthle (oncocytic) cell changes (metaplasia); occasional macros, Hurthle cells, follicular cells
- little colloid
Px: have higher risk of primary thyroid lymphoma
Subacute (de Quervain) Thyroiditis (ST)
Rare, painful enlargement of thyroid caused by granulomatous inflam or virus which can cause transient hypothyroidism
- FNA usually not necessary
Micro: hypocellular; strangely-shaped foreign body MNGCs (up to 100 nuclei!!!), lymphs, rarely see a granuloma
Tx: NSAIDs, roids if severe
- self-limited dz
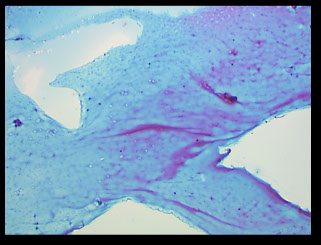
Reidel disease
Very rare; thyroid gets really hard 2/2 dense fibrosis
- presents as a diffusely enlarged, painless, firm thyroid
Micro: usually dry-tap on FNA but may see some fibrous tissue and inflam
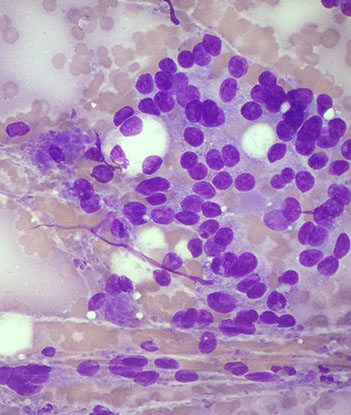
Follicular Neoplasm
- may also be called "Suspicous for a follicular neoplasm"; either way, lots of follicular cells are seen and the gland is coming out (lobectomy)
-- called "suspicious" bc cannot call (follicular) adenoma or carcinoma on cytology [people tried that and it didn't work out too well]
Follicular carcinoma is the 2nd MCC thyroid malig (up to 1/8); distinguished histologically from follicular adenoma 2/2 invasion of capsule and/or BVs
Cyto: lots of microfollicles c large crowded follicular cells, hypercellular, not too much colloid
Tx: lobectomy; then if malignancy found must do total thyroidectomy
Px: more aggressive than papillary ca
- likes to met to bones and lung, rarely to LNs
-- poor px if mets; excellent px if minimally invasive
Follicular Neoplasm, Hurthle cell type
-aka suspicious for follicular neoplasm, Hurthle (oncocytic) type; up to 4% of thyroid cancers
-- similar to carcinoma version of follicular adenoma (see above), capsular invasion defines malignancy and thus cannot be determined on FNA
Cyto: predominantly Hurthle cells that aren't cohesive and have a conspicuous nucleolus and lots of granular cytoplasm
- psammoma bodies often seen
IHC: (+) thyroglobulin and TTF-1
Genes: Hurthle cell neoplasms NEVER have PAX8-PPAR rearrangement (seen in 26-53% of follicular ca)
Px: 1/3 get LN mets
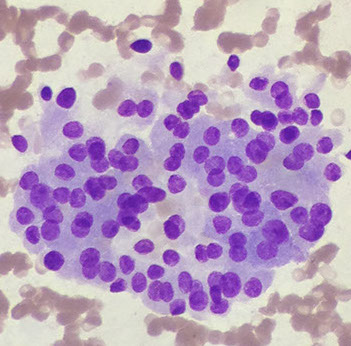
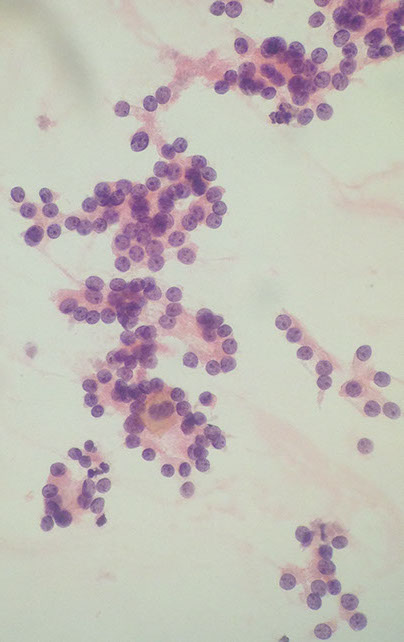
Poorly differentiated thyroid carcinoma (PDTC)
Rare (1/20 thyroid cancer), here cells are bwt a differentiated carcinoma (follicular, Hurthle cell, papillary) and anaplastic ca, but still represent up to 7/100 thyroid ca's; once again can only get definitive dx on histology
- most are dx'd as suspicious for neoplasm
3 patterns: solid, trabecular (ribbons), insular (nests c septae)
- all have microfollicles
Cyto: hypercellualr c dispersed cell c minimal pleomorphism (relatively monomorphous) c mits and necrosis
IHC: (+) TTF-1, PAX8
- Ki67 bwt 10-30%
Px: commonly have wide mets at time of dx
- 1/2 survival at 5 yrs
Anaplastic (undifferentiated) Carcinoma
Rare, one of the most lethal of all cancers causing 1/2 of all thyroid ca-related deaths but accounting for <5% of thyroid tumors
- rapidly growing mass causing hoarseness that spreads to adjacent structures by dx
- 1/3 arise from pre-existing cancer (ie papillary ca), thus these cancers may be a dedifferentiation of a preexisting differentiated thyroid ca
-F>M, 3:1
Cyto: large, hyperchromatic noncohesive cells c epithelioid or spindly shapes and marked pleomorphism c MNGCs
IHC: (+) CKs, PAX8
- negative TTF-1
- Ki67 >30%
Px: 5yr survival up to 1/8


Chronic lymphocytic thyroiditis
Subacute thyroiditis

Follicular neoplasm

Follicular neoplasm, Hurthle cell type
Anaplastic ca


Medullary carcinoma
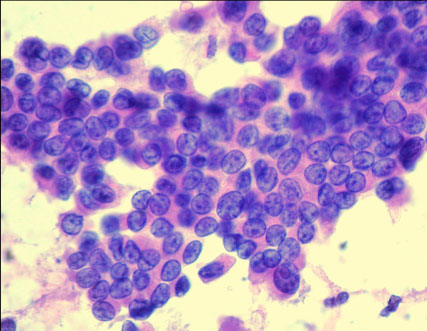
Up to 1/10 of all thyroid carcinomas that occur in 6th decade in 9/10, can be sporadic or AD
- arises from parafollicular (C) cells which make calcitonin
- assoc c MEN2a / 2b in ~1/5 cases
Cyto: Biphasic unform single / dispersed tumor cells or in loose clusters with epithelioid (round), plasmacytoid or spindled cells, lack of prominent nucleoli
Chromatin: Neuroendocrine (salt n peppa)
- mits seen in 1/8 cases
- red neurosecretory granules can be seen on diff quick that corresponds to calcitonin
- Amyloid blue blobs sometimes present
- has a small cell and a spindle-shaped variant
- may see intranuclear inclusions (not specific for follicular ca)
IHC: (+) Calcitonin, CEA, chromogranin, synapto, TTF-1
- negative thyroglobulin (bc derived from C cells)
- can see red granules on Romanowski stain
Genes: RET gene mutations (in 2/3), usually RETM918T
Px: 1/2 have regional LN mets
Medullary ca




Squamous metaplasia in PTC

Bubble gum colloid in PTC

Papillary thyroid ca (PTC)
MCC (4/5) thyroid ca in adult women up to menopause (and a little beyond)
- can present as a single distinct nodule
- can occur in any age group
- F:M 4:1, spreads via lymph
Micro: Papillary configurations; Pale powdery chromatin; Intranuclear pseudoinclusions and large nuclei c nuclear grooves ("Coffee Beans", caused by easily squishable nuclei); nuclei overlap and crowding common; psammoma bodies (not specific; seen in 1/2)
- Orphan Annie Nuclei are Optically clear, ground glass nuclei , are usually present histologically in papillary carcinoma (90% of cases), are artifacts of fixation, and cytologically nuclei look empty, devoid of chromatin with thickened nuclear membrane
- can have squamous metaplasia in PTC, septate vacuoles and bubble gum colloid
- also psammoma bodies and MNGCs
IHC: (+) keratins, thyroglobulin, TTF-1, PAX-8
Genes: 1/2 have BRAF point mutation usually (9/10) BRAFT1799A (V600E) val to glutamine; rest have RET/PTC1 and PTC3 rearrangement on 10q11.2, or RAS point mutations
- 1/20 have TRK rearrangement of NTRK 1 gene on 1q22
Tx: excision often curative
- may do subtotal thyroidectomy to leave some normal thyroid to support parathyroids
Px: excellent if excised
- BRAF point mutations assoc c poor px
Follicular variant of papillary carcinoma
Inc in freq (~1/5 of thyroid ca's)
- intraobserver agreement poor
- range of dx's and outcomes
- non-invasive fvptc appears b9
- encapsulated fvptc c capsular / vascular invasion has similar px as minimally invasive FTC
- non-encapsulated FVPTC has similar px as PTC
Reclassification?
May be non-malignant neoplasm, which would change performance of FNA and molecular testing
Parathyroid adenoma
May be mistaken clinically for thyroid nodules
Cytology: variablyt cellular c loose cohesive sheets, ribbonlike cords, occasional microacini,
- nuclei round c coarsely granular chromatin pattern; nucleoli small or prominent, and cytoplasm moderately abundant and granular
- nuclei can be more salt and peppery
- isolated cells and naked nuclei can be present
- focal nuclear pleomorphism can be present but is not prominent
- colloid is absent
Can be mistaken for follicular lesion of thyroid
- hypercalcemia is a clue for favoring parathyroid adenoma
Parathyroid adenoma
Metastasis to Thyroid
Renal, breast, melanoma, lung colon
Renal: moderate-high cellularity, single cells, papillae, sheets, clusters, lots of vacuolated or grnular cytoplasm
Breast: cellular, cells larger than follicular cells, lack of follciles, greater nuclear atyia and intracytoplasmic mucin
Melanoma: dishesive, plasmacytoid, spindled, anaplastic cels, INCIs can be seen, prigment can be present
