Thyroid and Parathyroid Endocrinology
Introduction
Parathyroid endocrinology
- Parathyroid disorders
Thyroid endocrinology
- Hypothyroidism
- Hyperthyroidism
- Thyroid function tests
Introduction
Endocrinology - The study of intra and extracellular communication by messenger molecules called hormones.
Hormones - Produced in an organ, but acts upon a distant location.
- Secreted into the blood prior to use
- Making circulating levels indicative of endocrine gland activity and target organ exposure
Interact with receptors in/on the target cell
Polypeptides / proteins
Synthesized and stored
Released into the bloodstream when needed by the body
Water soluble
Circulate unbound to carrier proteins or bound to them
Short half life
Examples, LH, FSH, TSH
Steroids
Produced by adrenals, gonads, & placenta
Synthesized by cholesterol but not stored by the body
Lipid-soluble
Circulate via carrier proteins and in the free form
Longer half-life
Free form is biologically active
Examples: estrogen, testosterone, progesterone, aldosterone
Amines
Have properties of steroids and polypeptides
Half-lives differ from very short to very long
Examples, epinephrine, norepinephrine, thyroxine
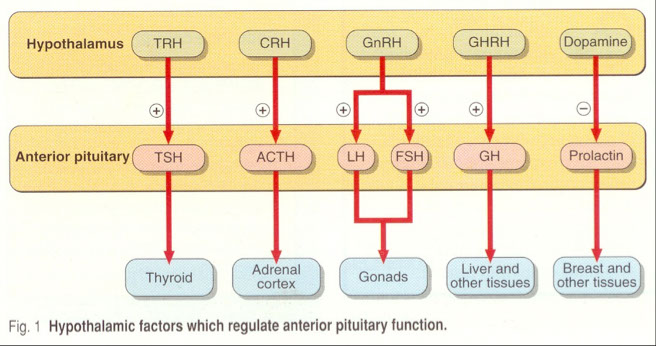
Components of endocrine system
Hypothalamus –
Produces stimulating & inhibiting hormones
Modifies & controls secretion of hormones from anterior pituitary
Occur in small quantities, therefore are measured by the response by the anterior and posterior pituitary
Pineal gland –
Produces melatonin
Controls circadian rhythms
Pituitary
Anterior – adenohypophysis
- Produces tropic hormones that regulate target glands
Posterior – neurohypophysis
- Releases hormones in response to suckling or changes in serum osmolality
Target gland or target cell
Disorder classification
Primary
Outside stimulating agents respond as expected
Hypo or hyper secretion of hormone from gland by its own volition
Glandular problem
Secondary
Target gland is functioning properly
Outside stimulating agents are in excess causing hypersecretion of the target gland hormone, OR
Outside stimulating agents are deficient causing hyposecretion of the target gland hormone
Tertiary
Problem at the hypothalmic level
Parathyroid Endocrinology
Role of the gland:
Regulate calcium levels
Chief Cells
-Most abundant
- Secretes parathyroid hormone (PTH)
Oxyphil cells
- Old chief cells
- Affinity for acidic dyes
Synthesized as a preprohormone (115 Amino a's)
Stored as prohormone (90 amino a's)
Released as an 84 amino acid molecule
- circulates with a half-life of 30 minutes
- Known as the intact molecule
Liver & kidneys produce two fragments from the intact molecule
Type of Parathyroid Hormone (PTH)
1) Intact PTH – circulating form
- All 84 amino acids
- Biologically active form
2) N-terminal
- Amino terminal end of the molecule
- 1 through 34 amino acids
- Biologically active
3) C-terminal
- Carboxyl end of the molecule
- 35 through 84 amino acids
- Biologically inactive
Mech: Regulates the amount of Ca in blood
- Normal: 8.8 – 10.4 mg/dL (2.2-2.6 mmol/L)
Regulates the amount of Ca in bone
- Controls bone density
Can live with ½ of a gland if necessary
More common to have more hormone from a hyperparathyroid gland
Hypoparathyroidism is less common
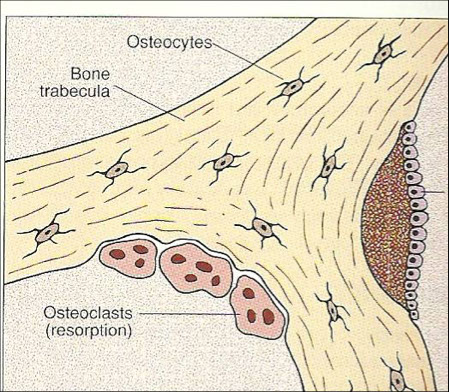
Calcium in bone
Ca combines with PO4 and forms hydroxyapatite
- Helps to form bone through osteoblastic activity
Osteoclastic activity releases bone Ca
Bone resorption results in ↑ Ca in blood
PTH directly causes Ca to be released from the bone into the blood
Calcium in serum
Controls normal conduction of electrical currents along nerves
Controls how nerves talk to one another
Controls muscle contraction
- Tingling sensations – low Ca
Controls normal brain function
- Brain feels “foggy” or confused – low Ca
- Feel run down or sluggish – high Ca
Forms of Calcium in Serum
Protein-bound – 45%
Complexed – 5%
Free or ionized – 50%
Serum proteins play important role
Adj Ca (mg/dL) = [Tot Ca (mg/dL ) - Albumin (g/dL)] + 4
Alterations in serum proteins will affect interpretation of results
Protein binding is pH dependent
Body requires more Ca during pregnancy
- Physiologic growth
- Lactation
Effects of pH on Calcium binding
Acid/base status causes fluctuations in ionized Ca levels
Acidosis
- H+ bind to albumin
- Less sites for Ca to bind
Alkalosis
- Fewer H+ to bind to albumin
- More Ca binds to protein
- Less free Ca in serum
Regulation
Ionized Ca concentrations control the synthesis and secretion of PTH
↓ Ca+ stimulate PTH secretion
↑ Ca+ inhibit PTH secretion
Additional factors:
Sudden ↓ Mg stimulate PTH secretion
↑ PO4 → ↓Ca → stimulate PTH
This is an INDIRECT cause of PTH secretion
Actions on target organs
Bone
Direct influence
Activates & ↑ osteoclastic cells
↑ mobilization of Ca
↑ resorption of Ca & PO4
↑ bone turnover rate
Kidney
Direct influence
↑ Ca reabsorption by distal renal tubules
↑ PO4 excretion
(↓ in serum)
↑ Renal α-hydroxylase activity
↑ conversion of
25-hydroxy Vitamin D to
1,25-dihyroxy Vitamin D
Vitamin D
Essential for maintenance of serum Ca
Absorbed thru the intestines
Formed in the skin by UV radiation
Becomes biologically active
Through metabolism
Cholecalciferol→25-OH-D3→1,25-(OH)2-D3
Liver→circulation→converted in kidney→active form
Intestine
Indirect influence
Increased levels of 1,25-dyhydroxy Vitamin D
-Enhances absorption of Ca in the intestine
- Stimulates osteoclastic cells in the bone
- Reabsorption of Ca in renal tubules
Calcitonin
Secreted by the “C” cells in the thyroid
Counteracts PTH
Lowers serum calcium
Inhibits osteoclastic activity
Inhibits renal tubule reabsorption
Increases excretion of Ca in urine
High levels of ionized Ca simulates release of calcitonin
Methodologies
PTH
2-site immunoradiometric (IRMA) assay
Measures the intact molecule
Very specific
No cross-reaction with PTH related peptide (PTHr)
Ca
Atomic absorption
Color-complex formation
Ion selective electrodes
Ionized Ca
Ion selective electrode
Requires collection on ice to reduce elevations in blood pH
Parathyroid Disorders
Associated with Hypocalcemia:
Ca levels fall below 8.5 mg/dL (2.25 mmol/L)
Tetany
CNS involvement
Hypoparathyroidism – rare
Accidental removal of the gland during thyroid surgery
Production of physiologically inactive PTH
Gland absent from birth
Pseudohypoparathyroidism – Ca remains low
Target organ resistance to PTH
PTH is elevated
Vitamin D deficiency - ↓ amounts of Vitamin D
Inadequate dietary intake
Malabsorption
Inadequate exposure to UV light
Rickets in children, osteomalacia in adults
Chronic renal failure – secondary hyperparathyroidism
Decreased synthesis of 1,25 (OH)2 D3
↓ Ca → ↑ PTH
Left untreated can lead to bone disease
Associated with diabetes
Associated with Hypercalcemia:
Ca levels are above 10.5 mg/dL (2.6 mmol/L)
Symptoms begin when Ca > 12mg/dL
Weakness, nausea, constipation, impaired mental concentration
Rehydration or drugs to ↑ renal excretion
Primary Hyperparathyroidism
Asymptomatic
80% are due to benign adenomas
PTH secretion is independent of negative feedback system
PTH is ↑ and Ca is ↑
Diagnosis is based on several serum Ca levels
Malignancy
Tumor directly invades the bone tissue
Some tumors produce PTHr
Causes osteoclasts to release bone Ca
PTH is inhibited
Toxicity
Example of too much of a good thing
Overconsumption of antacids
Excessive ingestion of Vitamin D
Thyroid Endocrinology
Synthesis of thyroid hormone
1. Active uptake of I- in exchange for Na+
2. Iodide may be discharged from the follicular cell by competing ions.
3. Iodide uptake is stimulated by TSH
4. Oxidation of iodide by H2O2 to form active iodine. - Thyroid peroxidase (TPO) catalyzes this reaction.
5. Active transport of iodine across cell membrane occurs.
Once thyroid hormone is released:
Binds to carrier proteins
TBG – thyroid binding globulin
- Binds T4 & T3
Transthryetin – pre-albumin
- Binds T4
TBA – thyroid binding albumin
- Binds T3
Circulate as free and bound forms
Dynamic equilibrium exists resulting in euthyroid status
T3 is the more potent and active of the thyroid hormone.
REMEMBER: Abnormal concentrations of binding proteins can result in abnormal total hormone concentration. ***** Remember this!
Mechanisms:
Regulates carbohydrate, lipid, & protein metabolism
Activates central nervous system
Stimulates heart & cardiovascular system
Regulates GI tract functions
Growth & development
Sexual maturation
Pregnency alterations of thyroid hormone by trimester
First trimester
Placenta produces large quantities of HCG
HCG stimulates thyroid gland to produce thyroid hormone (TSH-like effect)
Pituitary TSH decreases
Binding proteins increase
Second trimester
Binding proteins become saturated with thyroid hormone
HCG declines and pituitary TSH will begin to increase
Free hormone increases
Third trimester
When the binding capacity of the proteins is > hormone production from HCG stimulation
- Free hormone decreases
- Pituitary TSH increases
HCG – causes TSH-like effects
Binding proteins increase
Refer to the chart for comparison of T4, FT4, TSH, & TBG levels
Compare hormone levels by trimester
Explain the mechanism for hormone levels
Hypothyroidism
Fatigue
Slow mental performance
Cold intolerance
Impaired memory
Change in personality
Hoarseness
High cholesterol, LDL, Apo A & B, and increased risk for CAD*****
Primary Hypothyroidism disorders:
Myxedema – common symptoms worsen
Cretinism (congenital hypothyroidism)
Hashimoto’s disease (MC primary disorder)
Nodular thyroid disease – often benign
Subclinical – no apparent symptoms
Hyperthyroidism
Increased appetite with sudden weight loss
Fast heart beats/palpatations/tachycardia
Increased sensitivity to heat
Warm and clammy
Tremors
Increased anxiety and nervousness
Diffusely enlarged thyroid gland
Primary Hyperthyroidism disorders:
Thyroidtoxicosis – excessive thyroid hormones in circulation
Thyroid storm – life-threatening condition
Graves disease (MC primary disorder)
Thyroiditis
- Acute – usually caused by bacteria or parasite in an abscess
- Subacute – viral agent damages follicular cells
- Silent – autoimmune
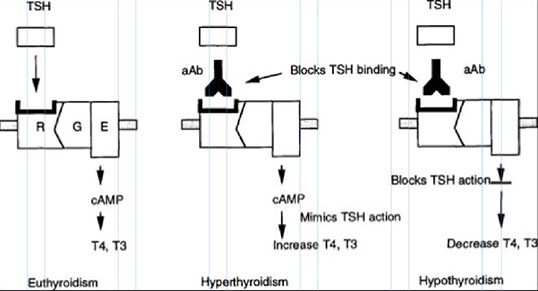
Mechanistic differences:
Hypo results in low thyroid hormone levels, hyper results in elevated levels
Hashimoto’s – a result of antibodies attacking follicular cells
Graves’ – a result of activated B cells attaching to TSH receptors on follicular cells
Thyroid Function Tests
TSH
Plays central role in thyroid’s economy
Inversely related to FT4
2-fold change in FT4 causes a 50-fold change in TSH
Earliest hormone to respond to thyroid gland function - *** best first test to get !!!***
Affected by many physiological states & drug interactions
Assay sensitivity essential to differentiating between hyperthyroid and euthyroid patients
Assay of choice is 4th generation
- 3rd generation assays detect 0.01-0.05 mU/L
- 4th generation detects to 0.001 mU/L
Interferences include:
Prior exposure of patient to mouse monoclonal antibodies
Presence of pituitary tumors – causes ↑ TSH but not because thyroid has stopped producing hormone
TRH Stimulation
Used mostly for identification of TSH secreting pituitary tumor or Thyroid hormone resistance syndrome
TSH measurements are taken prior to TRH administration for baseline level, followed by timed intervals
Normal response
- Rise in TSH, peaks 15-20 min, returns to base in 60 min
- Associated rise in T4 & T3
Free T4
Olden Days
- Critical step
-- Separation of free hormone from bound
- Gold standard method
-- Equilibrium dialysis
- Dilutions
-- NOT recommended
Immunoassay advantage
- Not affected by varying concentrations of binding proteins
Total T4
Serum levels are dependent on:
Rate of synthesis
Rate of release
Concentration of binding proteins
Peripheral conversion of T4 to T3
Methodologies
- Immunoassays
T3 Uptake
Assesses whether alterations in Total T4 are due to alterations of binding protein concentration or alterations of thyroid function
Resin uptake ratio (RUR)
RUR is inversely proportional to TBG, directly proportional to T3 present
RUR < 1, when BP is ↑
RUR > 1, when BP is ↓
RUR with TT4 to calculate FTI
Free Thyroxine Index (FTI)
Indirect measure of free hormone concentration
FT4I = T4 x T3U ratio
- Example: RR for T4 = 4 to 10 ug/dL
T4 = 12 ug/dL
T3 uptake = 25% (normal reference = 30%)
RUR = 25/30 = 0.83
FTI = 12 x 0.83 = 10 ug/dL
Compare the two results:
12 ug/dL without BP correction – outside of RR
10 ug/dL with BP correction – within RR
Total T3 and Free T3
TT3 most useful for confirming hyperthyroidism
Primarily reflects the hormone stores in the blood
Most useful for confirming early hyperthyroidism in patient with altered binding proteins
Free T3 assays have become better but still not widely used
Thyroid Antibodies
TSI – Thyroid stimulating Ig’s
TSH receptor Ab
Anti-TR
TRAbs
Anti-TPO
Thyroid peroxidase Ab
Formerly known as Anti-Thyroid microsomal Ab
Bind to follicular microsomal membrane
Fixes complement
Destroys tissue
Decrease in Thyroid hormone
Seen in 95% of patients with Hashimoto’s disease
Anti-Tg
Anti thyroglobulin Ab
TgAB
TRAbs (TSI)
Abs bind to cell membrane near/at TSH receptor site
Feedback system no longer works
Increased levels of thyroid hormone
Seen in 85% of patients with Graves disease















How Abs work
How TSI works

Anti-TPO