Small Intestines
Small Bowel Histology
Intro to biopsy
Artifacts
Reactive lesions
Hirschsprung's disease
Hernias
Duodenal ulcers
Amyloidosis
Autoimmune enteropathy
Behcet disease
Crohn disease
Pouchitis (see Colorectum)
Celiac disease (sprue)
Tropical sprue
Ulcerative Colitis
Microbe parade
Duodenal atresia
Adhesions
Lymphangiectasia
Malabsorption
Meconium ileus
Medication and Iatrogenic Injury
Microvillous inclusion disease
GALT deficiency
Intussusception
Ischemic colitis
Ischemic enteritis
Small Bowel Obstruction
Polyps
Carcinoma
Neuroendocrine tumors
Carcinoid tumors
Lymphoma and other heme lesions
Mesenchymal tumors
Other lesions
Peritoneum / Omentum
Mesenteric Cysts / Cystic lymphangioma
Multicystic benign mesoethelioma
Small Bowel
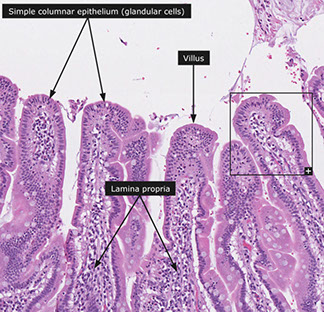
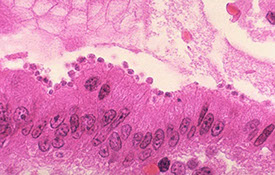
Small Bowel Histology
Proximal jejunum about twice as think and has double the diameter of the distal ileum, also has more prominent plica circularae.
- ileum surrounded by more fat and lies lower in abdominal cavity
- should eval bx in systematic fashion, noting first above the epithelium for orgs (Giardia) or presence of mucus (inc in CF), then if brush border present, if there are intraepithelial inflam cells (rare lymphs are normal), then lamina propria (may see tumor in lymphatics)
- surface epithelium can be bubbly / lipid-laden, with range of causes from lipid ingestion b4 procedure to abetalipoproteinemia; but should comment if hx of malabsorption
- PAS can highlight goblet cells and brush border
Layers of small intestines is pretty constant throughout:
1) Mucosa, 2) Submucosa, 3) Muscularis Propria, 4) Serosa
Mucosa
Plica circularae: Rings of mucosal-covered folds w/ submucosal cores that inc surface area and act as a barrier for shit movement
Layers of mucosa: 1- epithelium, 2- lamina propria, 3 - muscularis mucosae
Villi - projections of suface epithelium and lamina propria
- each villi covered w/ surface epithelium and has core of lamina propria w/ blind-ending lymph channel (lacteal), VAN and lymphos
Crypts of Lieberkuhn: tubular glands btw. villi that extend into muscularis mucosae
- interesting b/c Crypts of Lieberkuhn are depressions of the surface epithelium, whereas the villi are extensions of it. length ratio C:V- 3-5:1.
Epithelium of crypts and villi look similar (basal nuclei) but differ in function
- (+) CEA on apical surface of villi and crypt cells, in goblet cell mucin, and in glycocalyx.
-- CEA staining in cytoplasm anywhere is abnormal
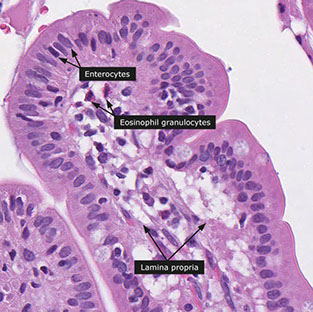
Villi: absorptive cell (columnar, eosinophilic cytoplasm) is major epithelial cell type found.
- brush border is PAS-(+) [from glycocalyx(which has important enzymes like peptidases and disaccharidases]
-- lack of glycocalyx may cause or result from milk allergy
Goblet cells randomly placed btw absorptive cells
- contain both acid and neutral mucin (stains w/ both PAS and Alcian blue)
-- small intestine has mostly sialomucins, whereas colon mostly has sulfomucins
- # goblet cells increases as move distally in small intestines
Endocrine cells also scattered in there, but rare; some lymphos too
Crypt: epithelial renewal is primary function (thus see inc mits)
- stems cells here give rise to all other epithelial cell types (absorptive, goblet, endocrine, and Paneth cells)
- Endocrine cells: called "open" if reach lumen (look pyramidal); or "closed" if don't reach lumen (appear more spindle-shaped)
-- may be easily ID'd b/c of eosinophilic infranuclear granules in cytoplasm (tho not always)
- Paneth cells: triangular-shaped; compose most of crypt base cells
-- have eosinophilic supranuclear granules (vs. endocrine cells)
-- may have some type of immune function
Lamina propria
on top of muscularis propriae, surrounds crypts, extends into villi
- separated from epithelium w/ PAS-(+) basement membrane
- made of collagen, CT, fibroblasts, mature fibrocytes, SM, and abundance of migratory cells, esp IgA plasma cells
-- occasional ganglion cells may be confused with CMV
Muscularis Mucosae
Made of elastic fibers and SM, delimits mucosa
- double layered
- extends through lamina propria into villi
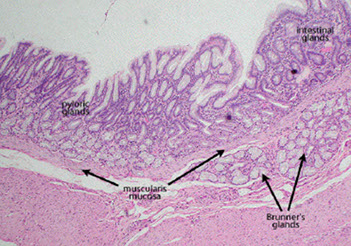
Submucosa
collagenous and elastic fibers with fibroblasts, with some migratory and fat cells
- major role in containing vessels that can go to either mucosa or down into muscularis propria
- Meissner's plexus found here, with neurons, (+)-neural stains
- Meissner plexus has neuronal cell bodies of the intrinsix sympathetic nervous sytem that work on local gut areas; it also has chemoreceptors and mechanoreceptors
Muscularis propria
Surrounds submucosa. Covered by subserosal CT and serosa
- outer long. and inner circular
- only a few dz's may cause fibrosis of this area (scleroderma ...)
- Auerbach's plexus found here!!!! has larger ganglia than Meissners
- Interstitial Cells of Cajal (ICC) found here
Serosa/ subserosa
Cuboidal mesothelial cells covering small bowel w/ thin band of CT underneath
Histo of small bowel longitudinal sections
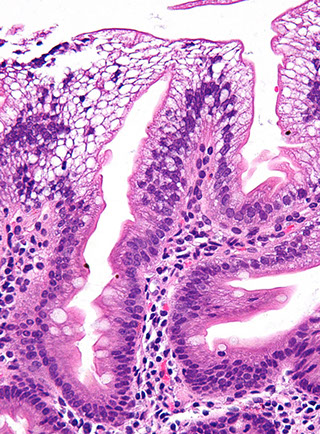
Duodenum
- difficult to tell GD junction on histo
- tissue subtypes:
1) mucosal/ antral/ pyloric type
2) villous absorptive type
3) transition btw other 2 types
- short fat villi
- highest conc of Brunner's glands (submucosal [vs intramucosal pyloric glands], cuboidal, light cytoplasm, tubuloalveolar glands, PAS-(+) cytoplasm, no goblet cells)
-- help to neutralize acid (?)
- pseudomelanosis duodeni: like melanosis coli but in duodenum and caused HTN, UGI bleeds, CKD, DM
Jejunum
- prominent plica circulares
- skinny, tall villi
Ileum
- connects to large bowel like cervical/ vag connection
- gradual loss of villi in transition to colon, w/ lots of fat in submucosa
- Peyer's patches in mucosa (some in submucosa)
-- Compartments: 1) follicle, 2) dome, 3) follicle-assoc epithelium, 4) interfollicular regions
-- most have germinal center w/ IgA-(+) B cells, CD4 Tcells, macrophages
---2) bwt follicle and overlying surface epithelium, w/ immune cells
---3) overlies lymph aggregates, diff. from villous epithelium b/c few goblets, lots of M cells (antigen-presenting cell w/ brush border)
Meckels diverticulum (remnant of omphalomesenteric duct) is the MC true diverticulum, which includes all 3 layers of the bowel wall and is a blind outpouchingthat communicates with the lumen
- usually occurs as a result of failed involution of the vitelline duct, which connects the lumen of the developing gut to the yolk sac
- solitary diverticulum extends from the antimesenteric side of the bowel
Rule of 2's ***
- found about 2 feet from IC junction, in 2% of pts, are 2 inches long, 2x MC in males (2M:1F), most often symptomatic by age 2 (though only 4% are symptomatic ever)
Gastric heterotopia: mucosal polyp in small intestine that has all cells present in normal gastric mucosa... pretty normal (in 2%)
- usually symptomatic and assoc w/ intussusception if distal to lig. of Treitz
Heterotopic pancreas also found sporadically thoughout DJI
Multilayering of crypts and/or oval-shaped glands generally means tissue cut tangentially
Hollande's fixative may preserve nuclear features better than formalin
Intro to biopsy
- reactive changes can be overlaying ca that was too deep to bx
- superficial portions of WDNT can be subtle, usually not assoc c inflam dz (as in the stomach)
- mets can mimic intraepithelial stuff if spread along sm intestine surface
- Pancreatic lesions can mimic sm bowel lesions when they arise from the ampulla
- must screen dilated lacteals for isolated cancer cells (mets MC from breast, lug, melanoma, and sometimes mesothelioma
- prominent crushed Brunner glands can look like neural tumors; but can avoid misdiagnosis by ordering PAS
- duodenum, and ampullary region are prone to reparative changes that can look like adenoma
Artifacts
Crushed Brunner glands - can look like nerve sheath tumors, spindle cell lesion, or Whipple Disease
Titanium flecks - little black specks seen in lymph aggs, from toothpaste or other food ingestion
Reactive Lesions
Small intestine can turn to gastric-type epithelium when injured (vs esophagus and stomach turning into intestinal epithelium) is called gastric mucin cell metaplasia
- this metaplasia may aid the growth of H pylori and can form nodules ( can cause changes suggestive of adenomas, but will stain c PAS, suggesting metaplasia and not dysplasia)
- gastric metaplasia in duodenal bulb not necessarily means Crohns dz, but should more consider Crohns if seen in terminal lieum (TI)
- may be overlying a ca that was too deep to bx, mimicking Crohns
Enteric mucosal calcinosis - seen c renal failure
Hirschsprung's disease
80% male, 10% c Down's syndrome
Aganglionosis of distal rectum that extends proximally causing a lack of propulsive peristalsis
- mostly short, <40 cm
Inc nerve fibers, mucosal acetyl cholnesterase activity and MHC II
Complication: Hirschsprung's Assoc EnteroColitis (HAEC)
Genes: RET gene
Hernias
Hesselbach's triangle
Lateral border of rectus abdominis; inferior epigastric artery and inguinal ligament
***MD's don't LIe *** Medial to inf epigastric A = Direct; Lateral to inferior epigastric a = Indirect ***
Direct Inguinal Hernia
Protrudes directly through inguinal (Hesselbach's) triangle and external spermatic fascia (only)
- bulges directly through abdominal wall Medial to inferior epigastric artery
- usually occurs in older men
Indirect Inguinal Hernia
Protrudes through INternal (deep) inguinal ring, external (superficial) inguinal ring, and INto scrotum
- enters internal inguinal ring lateral to inferior epigastric
Occurs in male INfants 2/2 failure of processus vagINalis closure
Femoral hernia
Leading cause of bowel incarceration
Bowel goes through femoral canal, which consists of inguinal ligament (superior), Adductor longus / pubic tubercle (medial) femoral vein / sartorius (lateral)
- MC in Females
*** generally in femoral anatomy, lateral to medial is NAVEL: Nerve, Artery, Vein, empty, Lymphatics
Diaphragmatic hernia
Abdominal structures enter thorax
- can occur in infants as a result of defective development of pleuroperitoneal membrane
- sliding hiatal hernia MC, where stomach slide up through esophageal hiatus of diaphragm, making an "hourglass stomach
Duodenal ulcers
90%+ occur in duodenal bulb
Pain dec w/ meals --> weight gain
~100% w/ H pylori infx
Due to inc gastric acid secretion (Zollinger-Ellison) or dec mucosal protection.
Brunner gland hypertrophy
Usually w/ clean, punched-out margins, as opposed to raised/ irregular margins of carcinoma.
Complications: bleeding, penetration into pancreas, perforation, obstruction (not necessarily precancerous)
Dx: Endoscopy
Tx: Triple therapy (2 abx + PPI)
- stop NSAIDs, aspirin, EtOH
Amyloidosis
GI tract almost always affected in systemic cases of amyloidosis, esp in stomach and rectum, can be patchy or diffuse
- amyloid can be deposited in any layer (mucosa to serosa)
- usually older pts that can have GI bleeding and other nonspecific sx (diarrhea, malabsorption)
Autoimmune Enteropathy
Has small intestinal villous atrophy that does not respond to dietary restrictions, unrelenting diarrhea, predisposition to autoimmune dz
- can affect any age
- may be 2/2 loss of self-tolerance and hyperactive immune system
- micro: may have inc CD4 and CD8 lymphs
- assoc c antigoblet cell ab and antienterocyte abs (both not specific)
the dz comes in 2 flavors:
1) Immune dysregulation, Polyendocrinopathy, Enteropathy, X-linked (IPEX) and is assoc c FOXP3 gene on X-chromosome which is expressed in CD4+ regulatory T cells
- fatal, assoc c lots of autoimmune conditions and prolonged diarrhea
2) Autoimmune Polyendocrinopathy-Candidiasis-Ectodermal Dystrophy (APECED) or Autoimmune Polyglandular Syndrome 1 (APS-1)
- AR, pts have severe enteropathy c hypoparathyroidism, adrenocortical insufficiency, DM, mucocutaneous Candidiasis, alopecia, vilitligo, and nail deformities
Behcet disease
Has oral ulcers, genital ulcers, eye lesions, some skin lesions and positive pathergy test
- deep penetrating ulcers can be seen throughout the GI (MC in TI esp assoc c Peyer patches)
Crohn disease
aka terminal ileitis, regional enteritis, granulomatous enterocolitis
- no known etiology; chronic relapsing dz that is multifocal and can be in any part of GI; classically in TI (rectum not usually involved)
- M=F in mid 3rd decade, familial assoc. presenting c crampy pain in RLQ, non-bloody diarrhea, fever, anorexia, can mimic acute appendicitis
- ulcers can cause bleeding, resulting in anemia
- fistulas and fibrotic obstruction of GI are main complications
- slight inc risk of adenoca
- endoscopy shows a multifocal process c apthous erosions, tram track / rake longitudinal ulcers, adjacent areas of normal mucosa, sometimes cobblestoning, strictures and fistulas
- may be confluent and involve entire bowel (add difficulty in dx)
- can see inflammatory polyps
- MCC of focal acute ileitis is medications (NSAIDS), not Crohn dz, thus establishing chronicity is critical
- pts on immunomodulation for Crohn dz can get variety of infx
Micro: gland destruction, apthous (aptha = spot) erosions with focal surface epithelial necrosis assoc c mixed chronic inflam and sometimes underlying lymph agg, see variety of chronicity of inflam processes, serpiginous ulcers, usually see focal cryptitis (neuts in crypts) adjacent to normal crypts
- transmural, so can have fissures, sinuses and fistulas
- normal submucosal vasculature lost (same as in UC)
- granulomas are rare, but if present are poorly formed and assoc c chronic inflam
- pyloric metaplasia seen c multiple bouts of inflam and repair (non-specific)
Pouchitis
see Colorectum
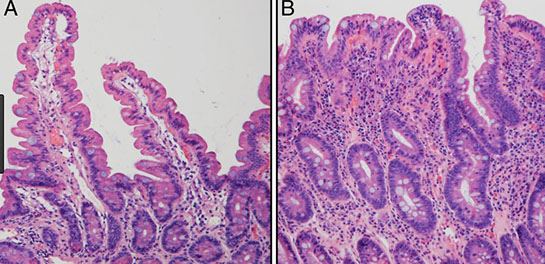
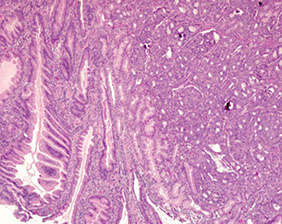
Celiac disease (sprue)
MCC malabsorption; ~1:100 prevalence in USA, esp. pts of Northern European descent, F>M
- HLA-DQ2 and HLA-DQ8, which lovingly present gliadin to Th cells (absence of HLA-DQ2 and DQ8 have high neg-predictive values)
- also HLA-B8 and HLA-Dw3 in 80-90%, also HLA-DQ2 and -DQ8
- commonly presents as anemia in pts >40 yrs
- pts get Fe def, folate def, anorexia, osteomyalgia, liquid poos, infertile, loss of height
- test for the sprue if pt has DM1 or unexplained high serum aminotransferases
- best to evaluate bx from beyond duodenal bulb, bc those are less affected by gastric damage
- Marsh classification used in grading celiac sprue
IgA autoantibodies against gluten (gliadin) [in wheat and other grains] and tissue transglutaminase (most specific), causing steatorrhea.
- IgG anti-tissue transglutaminase seen in pts c IgA deficiency
Assoc. w/ IgA nephropathy
- more prominent in pts c Downs syndrome and IDDM
-- other assocs: IgA deficiency, cystic fibrosis
Crypt hyperplasia and expansion of lamina propria (esp c plasma cells), villous atrophy (blunting), intraepithelial lymphocytes (IEL) (more prominent in the tips), dec. mucosal absorption, mucosal inflam
- these findings are non-specific, but number of IEL should dec at tips of villi; 6 IELs per 20 enterocyte nuclei at tip is too much
Mostly in proximal small bowel (jejunum)
- Inc lymphocytes --> inc risk of lymphoma
- 10% get dermatitis herpetiformis (Tx: Dapsone)
May classify c Marsh classification
Abnormal epithelial lymphocyte population (CD3+/CD8+) assoc c enteropathy-assoc T-cell lymphoma (EATL) and adenoca
- damaged villi can take years to grow back on gluten-free diet, and pts can still have lymphs after tx (correlate c serology in this case)
- villous atrophy can be seen in other dz's too (dermatitis herpetiformis, cow milk intolerance, giardia, peptic duodenitis, Crohns, SBBO, CVID, post-rads, lymphoma, malnutrition, ischemia, other sprues, amyloidosis)
Dx: IgA anti-tTG (tissue transglutaminase) is preferred test
- may also do antiendomysium ab, though more labor intensive
- may test for HLA-DQ2/-DQ8 (though is present in 1/3 of white people); very sensitive test (if its negative, you don't have celiac dz)
- if pt is IgA deficient, can do test for IgG
- anti-gliadin is not very sensitive or specific (prolly shouldnt be done; pts c Crohn dz can be anti-gliadin+ and have inc IELs, leading to misdiagnosis of sprue)
- small bowel bx needed to confirm (4 bx's from distal duodenum)
IHC: CD3 may over-highlight lymphs, leading to over-diagnosis of Celiac
Tx: Gluten-free diet
- may do a bacterial pre-digestion
DDx in refractory cases: enteropathy assoc T-cell lymphoma (EATL), pt not gluten free,
Px: have higher risk of getting ca (EATL)





Duodenum - Brunner's glands
TI - Peyer's patcht

Meckel diverticulum. The blind pouch is on the antimesenteric side of the ileum

Meckel diverticulum with ectopic gastric mucosa

Crushed Brunner glands can look like spindle cell lesion



Celiac disease
Tropical sprue
Most likely caused by infectious agent; seen in adults from tropics
- Responds to abx.
Similar to celiac sprue, but can affect entire small bowel.
Assoc. w/ megaloblastic anemia (poor nutrient absorption [give folate]; can also get B12, vits D, E, A, K deficient)
Ulcerative colitis
Sm intestine usually not affected, but can extend a short distance in, causing "backwash ileitis"
Microbe Parade!!!
Adenovirus
Marked lymphoid hyperplasia that can cause intussuception
Campylobacter
MC bacterial enteric pathogen; infx of colon, c watery or blood diarrhea in developed countries from poorly cooked chicken, milk, other foods (reservoir is chickens, sheep, cattle, pigs)
- can be sporadic or in children or travelers
- comma-shaped, flagellated, gram neg bugs; infx can be caused by ingestion of 500 organisms; 8 day incubation
- Micro: neuts in mucosa and intraepithelial, can have cryptitis and crypt abscess, although crypt architecture preserved
- can be complicated by Guillain-Barre or arthritis
Claustridium difficile
Infx of colon causing pseudomembranous colitis, seen in immunosuppressed or after abx tx (loss of normal bacterial fauna) causing watery diarrhea and fever
- can be complicated by relapse or toxic megacolon
- toxins released cause ribosylation of small GTPases, like Rho, causing disruption of epithelial cytoskeleton, tight junction barrier loss, cytokine release, and apoptosis
- can form pseudomembranes, made of layer of inflam cells and debris
- Micro: surface is denuded and has lots of inflam near surface c some fibrin thrombi in capillaries
- eruption of mucopurulent exudates looks like volcano
- diagnosed by finding C difficile toxin, not culture
- tx: vancomycin or metronidazole, possibly fecal transplants
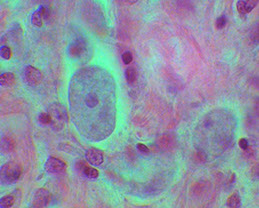
Mycobacterium avium-intracellulare
An opportunist in immunocomp (AIDS, CD4<100), spreads throught GI, can be prevented c clarithromycin and erythromycin
Found in lamina propria and regional LNs, but no granuloma (seen c TB)
Plump foamy macrophage or fibrillary cytoplasm
IHC: AFB/PAS+ intracytoplasmic mycobecteria
Parasites
>1/2 of the world gets chronic / recurrent infx
Ascaris lumbricoides
Nematode, in >1B ppl worldwide; eggs ingested hatch, penetrate gut wall going through blood to the lungs, maturing in alveoli then getting coughed up and swallowed returning to sm bowel and cause eosinophilic rxn
- may cause hepatic abscess or cause Ascaris pneumonitis
- dx made c eggs in stool
Strongyloides Stercoralis
Nematode native to Tennessee and Kentucky, rhabdotiform larvae in stool; short buccal cavity and bulbous esophagus
- filariform larvae penetrate skin or autoinfection from coughing and swallowing, where it matures to adult and reproduces (male leaves after mating but females can stay up to 3 decades or life!)
- after ingestion of eggs, larvae hatch in intestine and release larvae that penetrate mucosa causing autoinfx, does not need larval stage outside the human body
- Can cause Gram negative sepsis or meningitis during migration in immunocompromied pts
- should be tipped off to look if lots of eos, lymphs or plasma cells, or Charcot-Leyden crystals
- treatment c roids can lead to hyperinfx
Necator duodenale and Ancylostoma duodenale
Hookworms, 1B infected, larvae penetrate skin and develop in lungs and then swallowed, then attach to mucosa in sm intestine and suck blood, causing iron def anemia
- dx: eggs in fecal smear
Enterobius vermicularis
Pinworms, 40M infected in USA, live entire life in intestine, do not invade tissue, rarely cause serious dz, fecal-oral transmission
- eggs and adult pinworms viable outside human body
- egg deposition causes itching, scratching causes autoinfx through fecal oral route, adults come out at night, can use the tape test to get eggs
Trichuris trichiuria
Whipworms, do not penetrate intestinal mucosa, rarely cause serious dz, but can be complicated by prolapse; can cause bloody diarrhea
Schistosomiasis
adult worms live in mesenteric veins; eggs trapped in mucosa and submucosa cause sx, cause granulomatous rxn
Intestinal cestodes
Can be 2/2 Diphyllobothrium latum (fish tapeworm), Taenia solium (pork tapeworm), Hymenolepis nana (dwarf tapeworm)
- stay in intestines, from undercooked meats / fish c encysted larvae
- larva released and scolex attaches to intestinal mucosa
- D latum can cause B12 def
Spirochetosis
MCC are Brachyspira pilosicoli and Brachyspira aalborgi
- usually in the colonic epithelium, which can present c diarrhea, anal discharge, esp in immunosuppressed (HIV/AIDS), although it usually looks grossly normal
- Micro: see fringed, basophilic line on apical border of colonocytes, which can be highlighted c silver stains, PAS and alcian blue pH 2.5
Entamoeba histolytica
- Protozoan; aka infectious colitis or amebiasis
~ 10% of world population infected c E. histolytica, which is endemic in tropical places and may contribute to 100k deaths annually from diarrhea
- majority of pts asymptomatic, but shed cysts
Cecum > rt colon > rectum > sigmoid > appendix or TI
- can met to liver, and from there to brain; or can just stay in liver and cause a liver cyst / abscess (MCC in men, usually just a single cyst)
- can further go to heart, brain, kidneys
Cysts ingested from fecally contaminated food / water, or as STD
- cysts have chitin wall that are resistant to acid in stomach
Micro: amebas in lamina propria c necrosis w/o much inflam
- "flask" shaped ulcers
- trophozoited look like macrophages, round to oval c possible halo, abundant vacuolated cytoplasm that can have emperipolesis of RBCs
Dx: Stool for ova / parasites
- can see antiamebic abs and amebic ag in serum of pts c liver abscess
Tx: Metronidazole
Giardia duodenalis
Trophozoites and cysts
Giradia lamblia
aka G duodenalis or G intestinalis; described by Leeuwenhoek looking at his own poop; flagellated only need 10 cysts to infect; resistant to chlorine, thus endemic in unfiltered water
- secretory IgG and IL-6 can clear infx, but not in immunocomp or agammaglobulinemic pts
- pear-shaped, c 2 equal size nuclei, do not invade and sm bowel morphology may be normal, though can have inflam c heavy infx
Cryptosporidium parvum
Obligate intracellular, first described as cause of chronic diarrhea in AIDS pts, but can cause self-limited dz in normal pts
Oocysts in stool; can be killed by freezing (not found in Antarctica)
- infected 400k in Milwaukee in 1993
- sporozoites are motile and have special organlle to attach to vrush border and change enterocyte cytoskeleton
- causes nonbloody diarrhea
- only minimal histologic changes tho can have villous atrophy and crypt hyperplasia, mostly in terminal ileum and prox colon
- dx c oocystts in stool
Cyclospora cayetanensis
Obligate intracellular organism that spreads by fecal-oral route
Oocysts in stool
Escherichia coli
E coli Enterotoxigenic (ETEC)
Infx of sm intestine in developing countries causing severe watery diarrhea in infants, adolescents and travelers, from food or fecal oral route, no known reservoir
- can cause electrolyte imabalances and dehydration
- produces heat-labile toxin (LT) and heat-stable toxin (ST) which both induce chloride and water secretion and inhibit fluid absorption
- LT is similar to cholerat toxin and activates adenylate cyclase, causing inc intracellular cAMP, stimulating chloride secretion
- ST binds guanylate cyclase and inc intracellular cGMP causing transport effects similar to LT
Enteropathogenic (EPEC)
Infx of sm intestines seen worldwide from fecal-oral route c human reservoirs, causes watery diarrhea in infants
- can lead to dehydration and electrolyte imbalances
- make Attaching and Effacing (A/E) lesions where bacteria attach to apical cell surface and destroy microvilli; the protein is encoded by a large genomic pathogenicity island, the locus of enterocyte effacement (LEE) that is also present in EHEC, which also encodes a type III secretion system similar to Shigella
Enterohemorrhagic (EHEC)
Infx of colon which can be sporadic or endemic worldwide, causing bloody diarrhea from eating beef, or dairy, with widespread reservoirs, including cattle
- produce Shiga-like toxin, and outbreaks similar to S. dysenteriae infx, and O157:H7 can cause bloody diarrhea and HUS
- tx: should NOT use abx bc releases Shiga toxin which may lead to HUS
Enteroinvasive (EIEC)
Infx of colon causing bloody diarrhea in young kiddos from eating cheese, other food, water
- seen in developing countries, no known reservoir
- no known complications
- do not produce toxins, but invade epithelial cells and cause non-specific colitis
Enteroaggregative (EAEC)
Infx of colon causing nonbloody diarrhea, afebrile in kiddos, adults and travelers
- no known reservoirs, seen worldwide, mech of transmission not known
- attach to enterocytes c adherence fimbriae and helped by the bacterial surface protein dispersin, that neutralizes the negatice surface charge of LPS
- also produces other enterotoxins related to Shigella and ETEC ST, though damage is minimal
Histoplasma
Common in immunosuppressed (def INF-a), but can mimic Crohn dz in immunocompetent
- cause portal lymphohistiocytic inflam in liver, 1/5 get liver granuloma
Isospora belli
Found bwt adjacent enterocytes; football-shaped
Oocysts in stool
Microsporidia
Causes chronic diarrhea, often with dehydration and malabsorption
See subtle vacuolization of surface epithelium, endoscopy normal usually
- PAS and GMS; modified trichrome on fecal smear stains orange-red
- red band / dot often present
- DDx: Cryptosporidia, Cyclospora, Isospora, normal epithelium
Salmonella
S. typhi causes typhoid fever; S. enteritidis causes nontyphoid salmonella
- similar to Shigella, have type III secretion system to inject bacterial proteins into M cells which activates TLR5 that causes inflam
Seen worldwide, reservoir is poultry, farm animals, reptiles, may be transmitted by meat, eggs, poultry, dairy, to kiddos or older adults
- affects the sm bowel and colon, sx are watery or bloody diarrhea
- be lead to sepsis or abscess formation
Shigella
Human reservoir, seen worldwide, though endemic in developing countries, fecal-oral or contaminated water, in kiddos, migrant workers, nursing homes, travelers, affecting the left colon and ileum
- gram-neg unencapsulated, non-motile, facultative anaerobes, resembling E coli; infective dose is several hundred organisms (highly infective bc resistant to harsh acidic envts)
-- taken up by M (microfold) cells, which sample and present ags in intestine
- carry virulence plasmids causing type III secretion system that injects bacterial proteins into host cytoplasm
- sx: bloody diarrhea, can be complicated by reactive arthritis, urethritis, HUS, conjunctivitis; may be confused c chronic inflam bowel dz
- tx: antibiotics may help
Tropheryma whippelii
- causes Whipple disease
Infection with Tropheryma whippelii (gram positive), M>F white
- MC in middle-aged males; Giardia assoc (?)
- bx should be taken from prox and distal duodenum and jejunum
- partial tx may dec # of macrophages, and dz may be limited to heart or brain (not intestines)
- the malabsorptive diarrhea is caused by impaired lymphatic transport (lymphatic blockage)
Arthralgia, cardiac and neurologic sx. common
- Triad: Arthralgia, diarrhea, lymphadenopathy
Also Oculomasticatory myorhythmia
Micro: PAS-positive foamy macrophages in intestinal lamina propria and mesenteric LN c blunt round villi and dilated lacteals and lipid deposits
- the foamy macrophages have PAS+ diastase resistant stuff made of partially digested bacteria
- villous expansion is caused by dense foamy macrophage infiltrate giving a shaggy
EM: membrane-limited sac, full of dense spherical and rod-shaped bodies
DDx: MAI (AFB / PAS+)
Tx: 10 days of ceftriaxone, then 2 years of TMP-SMX
- f/u c PCR, not PAS
Typhoid (Enteric) Fever
Infx of sm bowel (Peyers patches of terminal ileum) seen in India, Mex, Philippines; human reservoir, fecal-oral or H2O transmission, causing bloody diarrhea and fever in kiddos and travelers
- may see rose spots, osteomyelitis in sickle cell pts, or other extraintestinal complications
- can result in chronic infx, carrier state, bowel perforation, encephalopathy, myocarditis
- typhoid nodules can be seen in liver
- blood cultures are positive in >9/10 pts during febrile phase
Vibrio cholera
Infx of sm intestine causing cholera, in India and Africa, can be sporadic, endemic, or epidemic
- see lots of watery diarrhea, from hours to 5 days after exposure to unsafe water/food esp uncooked seafood (shellfish reservoir)
- up to 100k deaths per year, from dehydration, electrolyte imbalance
Yersinia sp.
Yersinia enterocolitica and pseudotuberculosis cause GI dz; and Y pestis causes the plague
- invade M cells, using adhesins to bind host cell B1 integrins; pathogenicity involves capturing iron (those c hemochromatosis or inc non-heme iron at inc risk of infx)
- Infx of ileum, appendix, right colon in Northern and Central Europe; pigs, cows, puppies and cats are carriers; presents c abd pain, fever, diarrhea, can cause necrotizing granulomas, erythema nodosum or reactive arthritis
- usually detected on resections bc cause dz is deep
- can be seen accompanying Crohn dz
Viruses
Norovirus
ss-RNA, a Caliciviridae member; causes 1/2 of viral gastroenteritis worldwide, MCC acute gastroenteritis requiring medical attn in US, 2nd to rotavirus in causing severe diarrhea in kiddos
- may be from contaminated water, P2P transmission
- can be very problematic in immunocompromised, can cause chronic diarrhea in up to 1/5 renal transplant pts
Rotavirus
Encapsulated dsRNA, causes 1M deaths annually esp in kiddos
- vaccine is live-attenuated (cannot give to immunosuppressed)
- innoculum is 10 viral particles; damage 2/2 nonstructural protein 4 (NSP4) causing epithelial apoptosis, loss of absorption
Adenovirus
Common cause if diarrhea in kiddos and immunocomp
- epithel degen c villous atrophy and crypt hyperplasia
- 1 wk incubation period
Duodenal atresia
2/2 failure of small bowel recanalization, see bilious vomiting and epigastric distention
- assoc c Down syndrome
Dx: "Double-bubble" sign on abd xray is classic
Jejunoilieal Atresia
Assoc c Cystic Fibrosis
Adhesion
Fibrous tissue caused by reaction to recent surgery that can cause bowel obstruction
Common Variable Immunodeficiency (CVID)
Can have lymphoid hyperplasia or granulomas, but lack plasma cells and apoptosis in lamina propria cells, does have villous blunting (usually assoc c IELs)
- more susceptible to infx (usually very overt infx)
Severe Combined Immunodeficiency (SCID)
X-recessive, Defective cellular and humoral immune responses
- caused by mutation in common gamma chain (gc)
Micro: intestinal lamina propria devoid of lymphs and plasma cells with lots of vacuolated PAS+ macrophages in lamina propria
Lymphangiectasia
Priamry intestinal lymphangiectasia usually dx'd b4 3 yo
- pts have growth retardation c variable degree of GI complaints
- may have generalized edema in GI if severe enough
- tx c high protein, low fat diet
Malabsorption
Includes celiac dz, refractory sprue and collagenous sprue, IgA def, abetalipoproteinemia, Topical sprue and Sm bowel bacterial overgrowth
Celiac dz (discussed above)
Refractory Sprue
Present like celiac dz, but serology negative, that can show brief improvement on gluten-free diet temporarily, but then recurs
- show subcryptal chronic inflam, some c gastric metaplasia or acute inflam
- may benefit from gluten free diet and immunomodulation
- have HLA-DLQ2, - DQ8 phenotype
- 2 types: 1 (CD3/8+, no T-cell clonality) and 2 (CD3+, CD8-, T-cells clonal)
Collagenous sprue
- may be assoc c lymphoma (?)
- may benefit from roids or anti-tumor meds
IgA deficiency
pts mostly health, may see inc IgM (compensatory), , these pts can have giardia, nodular lymphoid hyperplasia, celiac dz, mild intolerance, IBD
- IHC shows reduced IgA-making cells
Abetalipoproteinemia
Rare, AR, absent apoB, essential in chylomicrons (deliver fat from sm bowel to blood), due to lack of ability to deliver fat to the submucosa
- comes from defective microsomal triglyceride transfer protein (MTP), low total cholesterol and triglycerides, present c failure to thrive, have defective fat-soluble vitamin digestion
- see Burr cells in PBS
Tropical sprue
Seen in pts returning from developing world, usually the tropics
- can see range of presentation, from relatively normal c functional abnormalities to fully symptomatic
- respond to folate and broad-spectrum abx
- probably has some microbial etiology
SBBO
- pts present c diarrhea, have altered gut motility
- can be 2/2 underlying medical conditions (DM) or acid-lowering meds
- micro shows variety, from normal to Crohn-lke
- Dx: sm bowel aspirate and quantitative cultures gold standard
Meconium ileus
Meconium plug prevents stool passage in a newborn c cystic fibrosis
Medication and Iatrogenic Injury
Ipilimumab
mAb against cytotoxic T lymphocyte antigen 4 (CTLA4) for tumor immunization
- can be erythematous to ulcerated on endoscopy
- micro shows lymphoplasmacytic expansion of laminia propria c inc IEL and lots of apoptotic bodies; and can also have cryptitis and glandular inflam
- IHC shows inc T lymphs
Mycophenolate acid (MPA)
Initially has lots of apoptosis (like GVHD)
- key is finding crypt apoptosis
- CellCept (mycophenolate mofetil) used for maintenance immunosuppression in solid organs
- abnormal to find >2 apoptotic bodies per 100 crypts
- correlation bwt blood levels and clinical toxicity is imperfect
NSAIDS
Assoc c sm intestinal mucosal damage
- can cause strictures leading to "diaphragm dz"
GVHD
Have secretory diarrhea, abd pain, and sometimes bleeding
- syndrome of upper GI GVHD is anorexia, dyspepsia, food intolerance, nausea, vomiting
- can be scored from Grade 1 (inc crypt apoptosis) to Grade 4 (total denudation of areas of mucosa)
Microvillous Inclusion Disease
aka microvillous atrophy, Davidson dz, familial microvillous atrophy
- uncommon, congenital (AR), prolonged intractible diarrhea in early infancy, MCC malabsorption in neonatal period
- usually poor outcomes and require small bowel transplant
- Micro: wall of sm intestine was paper thin c diffuse intestinal villous atrophy (blunting) w/o inflam rxn, apical microvillous inclusions of surface enterocytes (seen c EM), no evidence of infx or allergy
- PAS shows bright apical cytoplasmic blush (can also be seen c CD10 and CEA)
Tufting enteropathy
- variant c adhesion molecule defects that shows varying degrees of villous atrophy c low or absent mononuclear cell infiltrates in lamina propria and tufting of the epithelium (classic "teardrop" morphology)
- has deposition of laminin and HSPG in BM, inc expression of desmoglein
- may be assoc c consanguinuity
IHC: good initial panel may include CD10, EpCAM and chromogranin
Genes: mutations in EpCAM (causes loss of staining)
EM: highlights abnormal intercellular junctional complexes
Galactose-1-phosphate uridyltransferase (GALT) deficiency
Screened at birth, presents c poor feeding, jaundice, coagulopathy, ascites, and E coli sepsis
Intussusception
Telescoping of bowel segment into a distal segment which can cause ischemia and is 2/2 a "lead point" which drags bowel into other segment during peristalsis
- surgical emergency during childhood
- is cancer until proven otherwise if occurs in adults
- lead point can be caused by inflamed Peyer's patches secondary to viral infx
Ischemic colitis
Reduction in intestinal blood flow causes ischemia
- colon mostly supplied by celiac, superior and inferior mesenteric arteries
- has collateral system so that slow loss of blood can shift to use other system
Presents as pain after eating (which can lead to weight loss) in elderly
- commonly occurs at splenic flexure and distal colon
- may be caused by volvulus (twisting of the bowel loop around a mesenteric attachment
Ischemic enteritis
Usually caused by mechanical alterations (rather than vascular insufficiency, as seen in ischemic colitis)
- can be seen in pts c inoperable liver mets receiving Selective Internal Radiation S[heres (SIRS) which look like small black spheres in submucosal vessels
Small Bowel Obstruction (SBO)
Mechanical obstruction to intraluminal contents
***ABC's ***
Adhesions: 75% due to surgeries, treat c Lysis of Adhesions (LOA)
Bulge / hernia: 2nd MCC, must r/o incarcerated hernia (pt has sx of fever, shock, acidosis, peritoneal signs)
Cancer / tumors: MC is metastatic colorectal cancer
- in infants, MCC is intussusception
Dx: see distended loops of small bowel and Air-Fluid levels on upright films
- paralytic ileus mimics SBO
Tx: NPO, NGT, IVF, Foley

tufting enteropathy

Microvillous inclusion disease (microvillous atrophy)

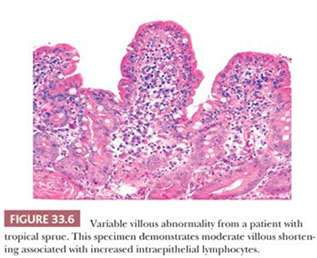
Tropical sprue


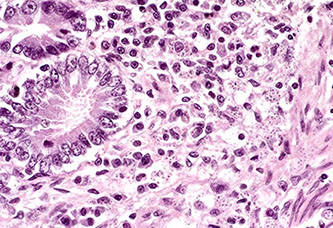
Campylobacteriosis in a pig small intestine



Disseminated Mycobacterium avium intracellulare complex (MAC) in Small Bowel


Ascaris lumbricoides
Ascaris lumbricoides egg




(Right) Duodenal biopsy showing Stronglyoides sterciralis larval infection in the mucosal crypts

Figure A: Longitudinal section of an adult hookworm worm in a bowel biopsy, stained with H&E. Note the oral cavity (OC) and strong, muscled esophagus (ES).


Hookworm egg in a wet mount

Enterobius vermicularis, pinworm

the smaller head of Trichuris embeds itself into the colonic mucosa (arrows below), leaving the larger body hanging


Schistosomiasis

Intestinal spirochetosis forming a thick filamentous band

Trophozoite of Entamoeba histolytica in a section of large intestine

Small Intestine. Intrahistiocytic yeasts (Histoplasma capsulatum) admixed with plasma cells in the lamina propria. 40X


Isosporiasis


Figure 5: Strategies that allow Salmonella spp. to cross the intestinal barrier, survive in intestinal tissues and spread systemically.
Microsporidia. small bowel biopsy shows numerous round plasmodial forms (arrow heads) in the apical cytoplasm of enterocytes, along with numerous intraepithelial lymphocytes (arrows)

Figure 4: Steps of Shigella spp. translocation of the intestinal epithelium and development of the infectious process leading to bacillary dysentery.

Figure 3: Steps of Yersinia spp. translocation of the intestinal epithelium and development of the infectious process leading to mesenteric lymphadenitis. [2]

Whipple disease
Whipple disease PAS

Whipple disease mechanism




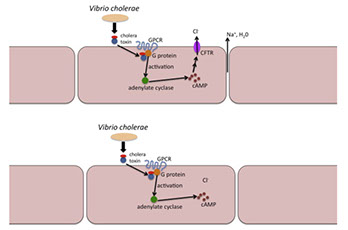
Top, cartoon of the mechanism of diarrhea mediated by Vibrio cholerae in intestinal cells from an individual with an intact and fully functional CFTR. The bacteria releases a toxin that constitutively activates an intracellular G protein, which consequently activates adenylate cyclase. Adenylate cyclase catalyzes an ATP→cAMP reaction and the product of this reaction eventually activates CFTR. The activated CFTR facilitates a chloride ion movement into the gut lumen, which causes an osmotic loss of sodium ions and water into the lumen. The net result is a watery diarrhea. Bottom, cartoon of the mechanism of resistance to Vibrio cholerae in intestinal cells from an individual with one or two alleles for the cystic fibrosis phenotype. As per the top panel, the bacteria releases a toxin, the G protein is activated, adenylate cyclase is activated and cAMP is produced. Because of the mutant allele(s) encoding the CFTR, there are either inadequate numbers or a complete absence of fully functional CFTRs to facilitate the chloride loss into the lumen.


Duodenal lymphangiectasia



Ischemic colitis

Ischemic colitis


Giardia trophozoites on mucosal surface
Cryptosporidium
Abetalipoproteinemia
Duodenal Waldenstrom macroglobulinemia

Polyps
Adenoma
Not very common in sm intestine, but usually in duodenum, usually solitary
- 3 histologic types: tubular, tubulovillous, villous
- endocrine cells prominent in pts c FAP (MCC death in pts c FAP after colectomy is upper GI tract malignancy (still req surveillance c capsule or endoscopic bx)
- usually malignant if in pts c FAP in the duodenum or stomach antrum
Micro: epithelial cells in true adenoma can absorb lipid but cannot process it, causing a lipid hangup at the surface (can be highlighted c PAS)
- initiation point just below surface of epithelium
DDx: reactive lesion (as in pts c peptic duodenitis c nodular configuration), which can have large dark nuclei, though there is also foveolar hyperplasia; and point of origin at base of mucosa
Tx: endoscopic papillectomy
Peutz-Jehgers Polyps
PJ pts get hamartomatous intestinal polyps in sm intestine (also have mucocutaneous skin pigmentation)
- have up to 70% risk of GI ca in lifetime
- PJ is AD, c complete penetrance
Micro: polyps are hamartomas and thus display morphology of their cell of origin; have arborizing sm muscle core from which mucosa leafs out
Genes: mutated LKB/STK11 in up to 19/20 PJ pts
Juvenile Polyps
B9 genetically heterogenous; can be limited to colon or generalized in GI
- some may classify as a hamartoma, or a b9 overgrowth of normal tissue
Micro: identical to Cronkhite-Canada polyps; except the flat mucosa bwt juvenile polyps is normal vs abnrml in CC polyps
- have edematous and inflamed lamina propria c dilated glands
Genes: some have AD mutations of DPC4/SMAD4 on 18q21
Cronkhite-Canada (CC) polyps
Rare hamartomatous polyp sundrome, mostly in Japan c diffuse polyposis throughout GI, except esophagus
- impossible to distinguish from juvenile polyp w/o clinical info
- flat mucosa bwt polyps is abnormal (vs normal in Juvenile polyps)
Micro: polyp c broad sessile base, expanded lamina propria, cystic glands
Tx: oral roids and nutritional support
Px: unclear if have malignant potential
Brunner Gland polyps
Unique to duodenum and reside in submucosa
ducts communicate to lumen opening in crypts bwt intestinal villi; make an alkaline mucus that neutralizes acidic luminal contents and protects mucosa from autodigestion
- Glands usually in tightly packed aggs c grey PAS+ cytoplasm and small basally located nuclei
- Brunners glands can normally be increased in reactive lesions (commonly c Chronic Peptic Duodenitis [CPD]), where can extend into lamina propria and cause the appearance of a nodule
- best to avoid the term "Brunner gland adenoma" bc do not normally produce dysplasia or ca
Brunner gland hyperplasia / hamartoma is a pedunculated polyp c Brunner glands and surrounding fibrous stroma that is usually >2 cm
- can present c intussusception, bleeding, or obstruction and can be large and well-defined
- Micro: submucosal-based mass c intact overlyingh mucosa c nests of b9 Brunner glands separated by sm muscle and vascular septa assoc c areas of cystic change
- larger polyps can produce sx of obstruction
Small lesions can be dx'd as Brunner gland polyp bc may be a hamartoma, or neoplastic
Crushed Brunner glands can look like neural or mesenchymal lesions; and a PAS highlights the bright pink Brunner glands
Gastric hyperplastic polyp
can herniate into prox duodenum (the bulb) that may cause clinical sx
- are edematous polyps lined c gastric foveolar-type mucosa, and can also have prominent sm muscle bands from prolapse
Carcinoma
Primary Adenocarcinoma (AC)
MC malig of sm GI (up to 1/2) but still rare (1/50) usually in older black men, usually sporadic, polyps are a risk factor, or several of the syndromes (highest risk c FAP), chronic inflam, ileostomy
- usually in periampullary region of duodenum, chance of being affected goes down as move more distal
Micro: simialar to other ACs; usually mod diff, up to 1/3 poorly diff
- degree of diff and special histo subsets (adenosquam, sarcomaatoid, mucinous) have little bearing on px (have usually invaded through wall at time of dx)
IHC: used to distinguish primary from met AC; are mostly CK7+ CK20+, though can also be CK7+ CK20- (vs CK7- CK20+ in colon AC)
Px: survival 1/3
Ampullary Carcinomas
Gland forming ca c intestinal or pancreatobiliary diff originating in ampulla of Vater (should only be used in ca's centered on the ampulla of Vater and not coming from adjacent organs)
- must assess for invasion
- should not overdx if any question or doubt in the site of origin (always put a note stating that tumor may have come from other places)
Micro:
- should search lacteals and BV for tumor cells
IHC: most CD20+, some (1/2) CK7+ (pancreatobiliary is CK7+ CK20 neg), CEA, CA19-9
Ddx: pancreatobiliary-type lesions have desmoplasia, incomplete lumina of cancerous glands c single gland of nuclei c 4x nuclear size differentiation, luminal necrosis in glands; intestinal type carcinoma is CDX2 and MUC2 + and CEA and CA19-9 +
Metastatic disease is 2x MC than primary ca in the small bowel
- usually melanoma, colonic AC, gyn or testicular dz
Neuroendocrine tumors
~1/3 sm bowel neoplasms, esp in blacks
- derive from foregut (duodenum) and midgut (Jej and Ileum); accounts for variable clinical behavior and NE differentiation
2nd MCC cancer in duodenum (usually in bulb); in older males; 2/3 make gastrin (1/3 of which get ZE), rest are somatostatin-producing (1/3 assoc c NF1) or D-cell tumors
- usually small polypod lesions (<2 cm) in submucosa
- prox sm bowel carcinoids almost never cause carcinoid syndrome
- rare small cell carcinomas (HG-NE tumors) usually found around ampulla and have poor px
In midgut, NE tumors usually are EC cell or serotonin-making, and usually found in ileum; and can produce carcinoid syndrome (1/20; these are the MCC of carcinoid)
- tumors more likely to be multicentric and large; usually found at more advanced stage and cause mesenteric fibrosis and obstruction
- midgut WDNT's malignancy is based on whether or not there are mets or not, rather than just histologic eval (clinically malignant tumors may not have pleomorphism, hyperchromasia or inc mits
Micro: WDNTs are monotonous prolif of small bland polygonal cells c mod amt cytoplasm; round regular nuclei and salt n peppa chromatin
- have variable architectural patterns (A = nested/insular; B = trabecular; C = acinar)
- D-cell tumors usually have prominent acinar growth pattern c intraluminal psammoma bodies
- HG-NEC, small cell type has prominent crush artifact and inc mits
Grading
G1 = <2 mits / 10 hpf or Ki67 <2%
G2 = 2-20 mits/10 hps, or Ki67 3-20%
G3 (HGNEC, small or lg cell types) = >20 mits/ hps or >20% Ki67
- survival determined in part by grade
Px: neg correlation c mets, tumor multiplicity, mits, invasion past submucosa and female gender; also size, depth and LN involvement
Lymphoma and other heme lesions
GI is MC location for extranodal NHL, and has most lymphoid tissue in body of any organ; MC are DLBCL and MALT lymphoma (usual type and those assoc c IPSID)
- inc risk c autoimmune dz, immunodef syndromes, immunosuppressive tx, Crohn dz and rad tx
Mesenchymal tumors
Smooth Muscle Tumors
Leiomyomas rare; either in mucosa or muscularis mucosa, can look like GIST (but diff IHC pattern)
- Leiomyosarcoma also rare
Inflammatory Fibroid Polyps
MC in stomach; uniform spindle cells, usually in submucosa, may cause intussusception if extension into lamina propria
- have lots of vessels, and can whorl around vessels (onoin-skinning), can have lots of eos
- can be edematous, liposarc
- have PDGFRA mutations and express CD34
GISTs of sm bowel
a rare dx; may not behave same as stomach GISTs
- GISTs in (2nd part) duodenum tend to bleed, have central necrosis if large, >1/2 have skenoid fibers (usually in small, less mitotically active tumors); malig potential related to size and mits, also coagulation necrosis, epithelioid histo, lack of hyalinized vessels and mucosal invasion
- GISTs in jej and ileum have same presentation, similar risk factors as in duodenum, although these behave 2x as poorly as gastric GISTs
- should consider NF if there are multiple tumors (works through RAS-MAPK pathway from NF1 inactivation)
IHC: to confirm should de CD117, CD34, sma, desmin, a keratin and S100
- express succinate dehydrogenase subunit B (SDHB; negative in syndromic [Carney triad] and peds; predicts treatment for imatinib)
Vascular lesions
Rare
- lymphangiomas can occur in kiddos in any part of sm bowel, exudes a milky substance when cut; micro shows lots of thin-walled lymphatic spaces filled c proteinaceous material ("lymphangiomatosis" is the term for diffuse lesions)
- hemangiomas rare, and assoc c Maffucci and Blue Rubber Bleb Necus Syndrome (BRBNS) have cavernous vascular channels filled c blood and surrounded by attenuated endothelial lining and sm muscle wall in submuosa and lamina propria
- angiosarcoma can be primary or met; grossly red, polypoid friable lesions, predominantly in submucosa, can have epithelioid morphology, expand through lamina propria and cause uleration; epithelioid cells can be positive for keratins and lead pathologist down wrong diagnostic path, except are neg for CD20 and strongly reactive for CD31, CD34 and FVIII; is aggressive
- Kaposi sarcoma; HHV8+, CD34+ spindle cells assoc c extravasated RBCs
Translocation Sarcoma
Tumors c genetic alterations tend to have uniform cells
- GI type clear cell sarcoma found in ileum of young adults, c sheets of uniform round to spindly cells, can be slightly nodular; S100+, neg HMB45; have EWS-CREB1 rearrangements (vs EWS-ATF1 in soft tissue); have overlapping features c NE tumors (+SYN, S100, neg keratins), can also overlap c melanoma, may need molecular testing
- rare fibromyxoid sarcomas have been present
Small Bowel Mesentery
Can have fibromatosis, inflam myofibroblastic tumor, sclerosing mesenteritis, calcifying fibrous pseudotumor
Mesenteric Fibromatosis
MC intrabdominal fibromatosis; is a slow growing mass in sm bowel mesentery, usually assoc c preg or Crohn dz
- esp prone to recur in pts c Gardnet syndrome, which is related to FAP (caused by APC gene mutations)
- can iniltrate through lamina propria into mucosa of GI
- grossly is firm c coarse white trabeculation that can look like a scar
- micro shows poorly defined and infiltrative margins c spindly fibroblasts separated by lots of collagen organized in parallel arrays
- scattered thin walled long compressed vessels seen in areas of hemorrhage, lymph aggs and calcification or chondo-osseous metaplasia; nuclei of cancer cells lighter than endothelial cells; low mits
- IHC: (+) actin
- neg CD34 and desmin
- may react c CD117 (usually weaker than in true GISTS, but can also do B-catenin stain if still doubtful)
Inflammatory Myofibroblastic Tumor (inflam Fibrosarcoma)
MC in childheed, arises in abdomen, involving various organs; can be solitary or multiple, micro shows fascicles or whorls of myofibroblasts c mod pleomorphism, rare mits; marked inflam infiltrate, usually plasma cells, but also lymph, neuts and eos
IHC: (+) SMA, CK sometimes, ALK (up to 7/10)
Genes: have ALK gene fusions at 2p23
Px: mostly indolent, but can be aggressive
Calcifying fibrous pseudotumor
- aka childhood fibrous tumor c psammoma bodies
- rare, b9 fibrous lesion; can be in adults when involves organs which can produce sx
- grossly well marginated but unencapsulated, white lesion
- micro: unencapsulated paucicellular hyalinized fibrosclerotic tissue c variable inflam infiltrate c lymphs and plasma cells, can have lymph aggs; psammoma bodies and dystrophic calcification seen throughout
- IHC (+) FXIIIa
- neg actin, desmin, FVIII, S100, neurofilament, CK, CD34, CD31
Other lesions
Xanthoma
Usually in stomach, rare outside; can be discrete solitary or multiple
- called "xanthomatosis" if infiltrative; and "tumorous xanthomatosis" if forms a mass
- may be assoc c hx of radiation; but not hypercholesterolemia
- can see xanthomatosis in sm bowel
- Micro: aggs of foamy histios w/o much fibrosis in the submucosa, muscularis propria and subserosa c rare involvement of mucosa
Gangiocytic Paraganglioma
Rare, majority found in duodenum (rarely in jejunum, pylorus or colon), in 6th decade; presents c abd pain, obstruction, bleeding
- grossly soft yellow cut surface c infiltrative borders
- Micro: 3 flavors of cells: (1) spindle cells that look like nerve sheath cells, (2) ganglion-like cells and (3) nested (endocrine-pattern) and papillary epithelioid cells
- IHC: (+) S100 (spindly sustentacular cells), SYN (ganglion-like cells) and NSE (all cell types); CKs (in 1/2), various hormones
- DDx: GISTs (have different S100 staining pattern)
- Px: b9; rarely met
Psammomatous somatostatinoma
Peutz-Jehger polyps

Duodenal PJP c characteristic arborizing muscle


Juvenile polyp c cystically dilated glands

cystically dilated glands and inflamed edematous stroma compatible with Cronkhite-Canada syndrome polyps (H&E, ×40)
Brunner gland hamartoma / hyperplasia




Clear cell sarcoma-like tumor of gastrointestinal tract is composed of uniform polygonal or rounded cells arranged in sheets with focal pseudopapillary or pseudoalveolar architecture. The well-defined nests of the clear cell sarcoma of soft tissue are not seen.
The cells have moderate amount of clear or lightly eosinophilic cytoplasm, centrally located round nuclei, and punctate or inconspicuous nucleoli. Basophilic macronucleoli of clear cell sarcoma of soft tissue are not seen. Mitotic activity is increased and necrosis is often present.
Most cases show osteoclast-type giant cells. The distribution of these giant cells is uneven and sometimes they are absent altogether. Touton type giant cells with peripherally located nuclei of clear cell sarcoma are not seen.
Psammomatous somatostatinoma
Peritoneum / Omentum
Mesenteric Cysts/
Cystic lymphangioma
Mesenteric cysts can be assoc c basal necus syndrome
- have round smooth, thin-walled cysts that can be filled c serous fluid or milky fluid if near jejunum (then called a chylous cyst)
- arise from lymph vessels and have smooth muscle in their walls
- called Cystic lymphangioma if large and multilocular
Micro: smooth muscle in cysts wall
IHC: (+) D2-40
Multicystic Benign Mesothelioma
aka Benign Multicystic Mesothlial Proliferation, Multicystic Mesothelioma of the Peritoneum
Rare, occurs in women of reproductive age in pelvic peritoneum, cul de sac, uterus, rectum
- hyperplastic reactive condition that is assoc c prior abdominal surgery, endometriosis, other inflammatory conditions
- grossly multicystic and filled c clear serous or gelatinous fluid and can be as large as 15 cm [3]
Cyto: benign sheets of monomorphic mesothelial cells [2]
Histo: multiple cysts lined by flat to cuboidal mesothlial cells which can be hobnailed
- can have reactive mesothelial proliferation in wall of cysts that can look malignant
IHC: (+) Calretinin, keratin
- negative FVIII
Px: up to 50% recur
DDx: lymphangioma (younger pts, chylous fluid in cysts, lymphoid aggregates and sm muscle in walls), other mesenteric cysts (usually unilocular), cystic teratoma (has fat and calcifications) [1]
Multicystic Benign Mesothelioma



References
1. Histology from: https://www.proteinatlas.org/learn/dictionary/normal
2. Sansonetti P. War and Peace at Mucosal Surfaces. Nature Immunol. https://www.nature.com/articles/nri1499
