Salivary Gland Cytology
Anatomy / General
Acute sialadenitis
Chronic sialadenitis
Granulomatous sialadenitis
Lymphoepithelial sialadenitis (LESA)
Sialadenosis
Benign cysts
- squamous cysts
- mucinous cysts
- retention cysts
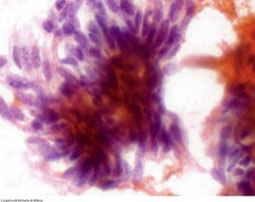
Pleomorphic adenoma (PA)
- Myoepithelioma
Basal cell adenoma
Oncocytoma
Warthin's tumor
Mucoepidermoid Carcinoma (MEC)
Acinic Cell Carcinoma
Adenoid Cystic Carcinoma
Basal Cell Adenocarcinoma
Clear Cell Carcinoma, NOS
Epithelial-Myoepithelial Carcinoma
Mammary Analogue Secretory Carcinoma (MASC)
Malignant Mixed Tumor
Myoepithelial carcinoma
Oncocytic carcinoma
Polymorphous low-grade adenocarcinoma (PLGA)
Salivary Duct Carcinoma
Primary Small Cell Carcinoma
Squamous cell carcinoma
The Salivary Gland FNA
effectiveness of cytomorphology alone:
sensitivity: 86-100%; specificity: 48-94%
- accuracy of b9 vs malignant: 81-100%
- combined FNA and RFS: sens 90%, spec 100%, accuracy 95%
Guide to management:
-Non-neoplastic - clinical FU
-B9 tumor/ low-grade carcinoma - limited resection
-metastatic dz to parotid LN - LN resection
-lymphoma - heme-onc referral
-high grade primary carcinoma - radical resection / nerve sacrifice / LN dissection
Milan System for Reporting Salivary Gland Cytopathology
I. Non-Diagnostic
- insufficient quantitative or qualitative cellular material to make cytologic dx
- 10% maximum rate
- min of 60 lesional cells for adequacy
Exceptions to non-diagnostic: atypia, tumor matrix, or mucinous cyst content
II Non-neoplastic
- inflam, metaplastic and reactive
- reactive LN (flow cytometry needed)
- clinico-radiologic correlation is essential to ensure the specimen is representative of the lesion
- a subset will need surgical excision to exclude the possibility of a poorly sampled neoplasm
III. Atypia of Undetermined Significance (AUS)
- cannot entirely exclude a neoplasm
- heterogeneous category
- majority will be reactive atypia or poorly sampled neoplasms
- specimens are often compromised (eg, air-dried, blood clot)
- Limited use (<10% of all salivary gland FNAs)
IV. Neoplasm
IVA. Neoplasm, benign
- reserved for classic benign neoplasms
- category will include conventional cases of PA, WT, lipoma, schwannomas, etc...
- ROM <5%
IVB, Neoplasm, salivary gland lesion of uncertain malignant potential (SUMP)
- diagnostic of neoplasm, however, a diagnosis of a specific entity cannot be made
- malignant neoplasm cannot be excluded
- many benign neoplasms and some low grade carcinomas
- ROM is 35%
Cellular Basaloid neoplasm
Cellular Oncocytic / Oncocytoid neoplasm
Cellular neoplasm with Clear Cell Features
V. Suspicious for malignancy
- aspirates which are highly suggestive of malignancy but not definitive
- often high-grade carcinomas with limited sampling or other limitation
VI. Malignant
- aspirates are diagnostic of malignancy
- sub-classify into specific types and grades of cancer
- grading is critical for clinical management
- "other" malignancies such as lymphomas, sarcomas, and mets are also included in this category and should specifically designated
Ancillary Studies
IHC (LBP, smears, FFPE)
FISH
RT-PCR
NGS
Risk of malignancy and treatment strategy for the Milan system
http://pathologycast.com/the-milan-system-for-reporting-salivary-gland-cytopathology-an-update-with-fna-examples/


b9 salivary
Reactive LN

Chronic sialadenitis

Mucinous cyst contents only, AUS. Turned out to be mucoepidermoid carcinoma

Pleomorphic adenoma

Warthin tumor, with oncocytes, background cyst debris, and chronic inflam

SUMP

SUMP. Basaloid neoplasm

ddx: basal cell adenoma, cellular PA, AdenoCa
Suspicious for malignancy, turned out to be epithelial-myoepithelial carcinoma


Salivary duct carcinoma, AR and HER2 positive
Anatomy / General
Salivary glands are protective and digestive in function: moisten mouth and help in swallowing, digsts carbs c ptyalin (amylase)
- controls bacterial flora c lysozyme
- souce of Ca2+ and phosphate for tooth development and maintenance; and have immunologic function (IgA)
Parotid (near ear) – Stenson’s duct
- has serous acini; proteins stored in zymogen granules
Submandibular (beneath the jaw)
-Wharton’s duct
- has seromucinous acini
Sublingual drains (beneath the tongue)
-Bartholin’s duct
- has mucinous acini; mucin stored in mucinogen granules
Minor salivary glands: scattered throughout mucosa of nasal and oral cavities, larynx and bronchial tree
- most abundant in posterior hard palate
Ectopic salivary glands: MC in periparotid and intraparotid LNs
Any new salivary gland mass should be FNA'd
- contraindications are pts c bleeding disorder, acute sialadenitis
- 4/5 tumors are either PA or WT
- 4/5 parotid tumors are b9, but 4/5 sublingual or minor salivary tumors are malig
Serous glands are PAS+, c pyramidal shaped cytoplasm that is foamy to coarsely granular, small bland eccentric nuclei, with or without small nucleoli, and naked nuclei are common
- mucinous glands are columnar in acinar arrangements, c small bland nuclei c small nucleoli
Ductal cells are in cohesive sheets or tubules, cuboidal to stratified columnar, small bland oval nuclei with or without small nucleoli, scant cytoplasm and delicate to abundant and squamoid; oncocytic metaplasia common
Myoepithelial cells - contractile function and used in production of basal lamina
- rarely identified in non-neoplastic salivary gland tissue (small dark nuclei overlying acinar clusters)
- usually identified in neoplasms (PA< ME) and can be spindle, stellate, plasmacytoid, or epithelioid
Oncocytes have large round nuclei, finely granular chromatin, prominent nucleoli, abundantly granular cytoplasm 2/2 mitochondria
can be:
- non-neoplastic (oncocytic metaplasia): normal (inc c age), chronic sialadenitis, oncocytic hyperplasia, benign lymphoepithelial lesion, Sjogren syndrome
- Neoplastic - Warthins tumor, oncocytic neoplasms, PA, mucoepidermoid ca, adenoid cystic ca
Hypercellular = malig
Inflam = sialadenitis and cystic lesions
Inc lymphs = lots of stuff
Mucin = MEC, mucocele, retention cyst, metaplasia
Chondromyxoid matrix = PA
Stromal spheres = adenoid cystic ca
Flower crystals = tyrosine crystals
Needle crystals = amylase crystals
Not all lesions require excision
- high grade lesions need radical excision, low-grade more conservative; easily distinguished by cytology
Core bx has higher risks of infx, damage to surrounding structures, pt discomfort / pain, needle tract seeding
- 1/10 have some tumor infarct after FNA
- RFS best for basaloid lesions (which can be either an b9 adenoma or carcinoma)
Cystic lesions (WT, MEC, acinic cell ca) have higher probability of false-neg and false-pos
Romanowsky stains good for seeing stroma and for lymphoid lesions
Pap stain good for seeing nuclei
Problems c FNA: wide variety of lesions; most b9 lesions very subtle, subtle differences bwt malig tumors
Normal aspirate is hypocellular with round groups of mucinous acinar cells with vacuolated cytoplasm, flat sheets and tubules of ductal cells and fat cells
Acute sialadenitis
Pt presents c diffuse glandular enlargement and tenderness (MC in parotid)
Acute inflam (neutros and necrosis), sometimes caused by sialolithiasis, but can also be 2/2 bacterial infx (staph or strep), CMV or mumps (viral acute onset can become chronic inflam)
- rare ductal cells
Micro: neuts and histios, few reactive / degenerative glandular cells, fibrin, debris and possibly calculi
Chronic sialadenitis
Firm, diffusely enlarged gland that mimics neoplasm (MC in submandibular gland), usually unilateral
- may be 2/2 duct obstruction cuased by stones, radiation, immunologic disorders, or infx
- FNA usually painful c scant cellular material (paucicellular c few acinic cells), can have reactive ductal cells, variable chronic inflam (lymphs), stromal fragments (fibrous tissue), proteinaceous debris
Granulomatous sialadenitis
Cuased by variety of infx (TB, fungi, calculi, sarcoidosis, bacteria), some tumors (Hodgkins, metastatic SCC, T-cell lymphoma), usually occur in upper cervical LNs, though can be seen in salivary



oncocytes

Acute sialadenitis
chronic sialadenitis

Chronic sialadenitis

Granulomatous sialadenitis
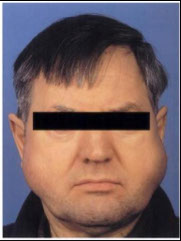
Lymphoepithelial Sialadenitis (LESA)
- aka Sjogren dz (systemic) & Mikulicz dz (local), myoepithelial sialadenitis, benign lymphoepithelial lesion
MC in women, presents c bilat parotid enlargement
- destructive lymphocytic infiltrate of salivary and lacrimal glands, c preservation of ducts and proliferation of myoepithelial cells
- dx suspected on hx and nature of inflam rxn
Hypercellualr c mixed inflam (small lymphs, plasma cells, and macros)
- lymphs can be in germinal center arrangement or in myoepithelial islands in a polymorphous lymph infiltrate
- assoc c HIV?
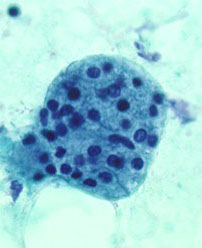
Sialadenosis
Refers to b9 nonneoplastic noninflammatory swelling in association with acinar hypertrophy and ductal atrophy. Usually bilateral parotid gland involvement (looks like a chipmunk)
- wide variety of causes
Aspirates appear normal except acinar cells are significantly larger than normal and inflammatory cells tend to be absent
- looks like normal cells "magnified"
Benign cysts
Squamous Cysts
Lined by squamous cells, this group of b9 cysts includes, congenital (branchial cleft and dermoid) cysts, simple lymphoepithelial cysts, and HIV-assoc cystic lymphoepithelial lesions
- presents as bilateral swelling c multiple cysts, surrounded by lymphoid tissue
Micro: in clear to turbid cyst fluid see hypercellular aspirate c macros, anucleate squames, c background of keratinaceous debris, mixed lymphs, clusters of squames or columnar cells, no lymphoepithelial islands (except HIV-assoc dz and cystic LESA)
- ddx: cervical cysts
Mucinous Cysts
Includes malignant neoplasms (MEC), inflam dz, and acquired cysts (mucoceles [pseudocyst bc no epithelial lining] and retention cyst [has lining]
Micro: Hypocellular c lots of mucin, histiocytes (muciphages), scattered inflam, amylase (needle-shaped) crystals
Retention Cyst
True cyst c epithelial lining, which can be 2/2 duct obstruction (sialoliths)
Micro: low cellularity, macrophages and few inflam cells, degenerate epithelial cells
Pleomorphic adenoma (PA)
B9 mixed tumor, MCC salivary gland tumor (1/2-3/4 of all salivary gland neoplasms), painless, firm mass usually growing slowly in tail of parotid at jaw angle
Micro: fibromyxoid background, epithelial (round to columnar cells c uniform round nuclei grouped in honeycomb pattern with frayed edges) and myoepithelial / mesenchymal (myxoid ground substance-secreting single cells that can be spindly, clear, plasmacytoid or epithelioid) cells c chondromyxoid matrix (looks blue like mucin / troll hair) and sometimes tyrosine crystals
- matrix component can be little or appear adenoid cystic
- 1/5 have atypia or metaplasia
Genes: (+) PLAG1 gene alterations pathognomonic
Myoepithelioma
Rare, B9, monomorphic version of PA (only has ME cells and lacks ductal differentiation)
Micro: only spindly myoepithelial cells c wispy cytoplasm or plasmacytoid c dense hyaline cytoplasm (no groups of epithelial cells as in PA, though can look epithelioid c glycogen accumulation), no chondromyxoid matrix, tho can have myxohyaline stromat
Basal cell adenoma
aka monomorphic adenoma
- cannot distinguish clinically from PA; MC in parotid
- has mostly epithelial cells and no fibromyxoid stroma through can hav hyaline material, has various histologic growth types (solid, tubular / trabecular, papillary, and membranous)
Micro: smaller basaloid cells c inc NC ratios and scant cytoplasm in groups / cords / irreg clusters / singly c peripheral palisading in a thick nonfibrillary stroma
- squamous whorls specific though rare finding
- can have metachromatic hyaline (dark pink) stuff
Dermal analog tumor (aka membranous type basal cell adenoma) has prominent component c spheres of matrix material
- can be confused c basaloid SCC or cylindroma
Oncocytoma
Rare, b9, up to 3% of all salivary gland tumors; MC in parotid of older pts; similar to Warthin tumor, but lacks lymphoid component; firm to palpation (not soft like Warthin tumor)
Gross: partial fibrous capsule, well demarcated
Micro: lots of polygonal oncocytes in clear background w/o lymphs
IHC: (+) PTAH
- negative diastase-resistant PAS (vs acinic cell ca)
Warthin tumor
- aka Cystadenolymphomatosum or adenolymphoma
Possibly derived from salivary duct remnants trapped in salivary gland LNs; feels doughy
- 2nd MCC salivary gland tumor (up to 1/10 of all)
- 1/10 are multifocal or bilateral
- inc risk in smokers
Micro: oncocytes (abundant granular orange to blue cytoplasm arranged in flat sheets / papillae) scattered and in groups c lymphs and granular debris in background that looks like it contains motor oil
- background nucleated and anucleated squames can be in atypical forms
Tx: resection c preservation of facial n.
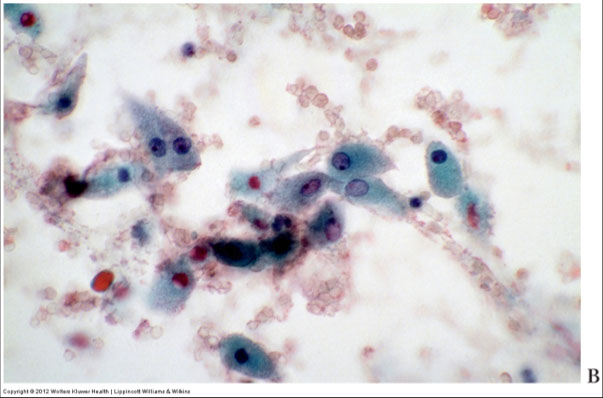
Mucoepidermoid Carcinoma (MEC)
MC (minor and major) salivary gland malignancy in kids and adults; usually in parotid and sometimes in palate or buccal mucosa; in 6th decade, but can be all ages
- low grade tumors are more cystic and present as painless soft cystic mass (commonly recurs); FNA shows bland mucus-producing glandular cells, muciphages, cyst content and lots of mucoid material
- higher-grade tumors are more solid and infiltrative c more sx (skin changes, pain, nerve damage) c FNA showing obviously malignant cells similar to non-K SCC, and glandular cells and intermediate cells c rare mucus and possible necrosis and mits
Cyto: Single and loosely grouped pleomorphic mucinous (glandular) cells found in low-grade tumors are cuboidal to columnar c irreg nuclear contours, coarse and clumped chromatin and prominent nucleoli and can be similar to muciphages, goblet cells or signet-ring shaped c lots of mucin;
- intermediate cells present in both low and high grade are relatively small c inc NC, small round nuclei, vesicular chromatin, inconspicuous nucleoli, and look like metaplastic squames or glandular cells, similar to reactive ductal cells
- high-grade tumors have lots of squamoid / epidermoid cells (hyperchromatic nucleus and dense orangeophilic cytoplasm) and intermediate cells that are bland and smaller c less cytoplasm
- mucin present in background
- clear cells present often
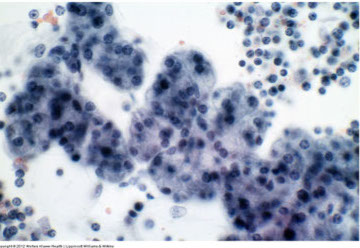
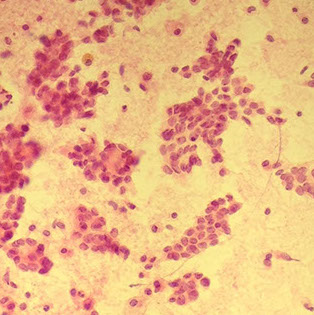
Acinic cell carcinoma
2nd MCC salivary gland malignancy in minor salivary glands in adults (up to 6% of all neoplasms and 1/5 malignancies); usually in the parotid gland of women in the 5th-6th decade
- well-circumscribed, slowly growing mass that is occasionally painful
Cellular smears c loosely cohesive polygonal bland serous acinar cells c eccentric nuclei in background of naked nuclei and lymphs
- abundant granular / vacuolated cytoplasm c indistinct cell borders, round uniform nuclei and small nucleoli c cytoplasm that is foamy to coarsely granular +/- psammoma bodies
- BVs can be seen in some clusters (perivascular tumor growth)
- may have intranuclear pseudoinclusions
- mits are infrequent
IHC: cells have PAS-(+) diastase-resistant zymogen granules in cytoplasm, keratin, alpha-1-antichymotrypsin, alpha amylosa, VIP, myoep markers, can have focal NE staining
Px: usually has late recurrences
DDx: normal parotid gland (tumors lack striated and interlovular ducts, lack lobular architecture)
Adenoid Cystic Carcinoma
MC in minor salivary glands, though is the 3rd MCC salivary gland neoplasm overall
- assoc c perineural invasion that can cause pain or paralysis
Cyto: variable sizes though usually large 3D acellular hyaline matrix globules and linear branching c sharp borders
- basaloid cells present that are small dark and uniform surrounding dense pink hyaline globules (bubble gum balls) that can be in clusters, tubules, cribriforming or single, may have focal atypia
- there exists a solid variant c lots of basaloid cells and scanty matrix
IHC: (+) duct cells - keratin, CEA, alpha-1-antichymotrypsin, S100, CD117 / c-kit
- (+) cells around pseudoglandular spaces: S100, actin, variable keratins
Genes: MYB protein overexpression in absence of detectable translocation
Px: protracted clinical course c poor long-term survival
Basal Cell Adenocarcinoma
Low-grade malig, rare, seen in up to 2% of salivary gland malignancies; usually in parotid, 7th decade; MC in parotid,
Cyto: identical to basal cell adenoma
- only distinguished by infiltrative growth
Px: Good, except has tendency to recur
Clear Cell Carcinoma, NOS
Prominent clear cells component, that can be 2/2 a number of things (fat, glycogen, mucin, etc etc)
- has a broad ddx
Epithelial-Myoepithelial Carcinoma
3/4 occur in parotid gland, 1% of salivary gland neoplasms; usually in women, has broad age range
- made of small inner duct lining cells and larger peripheral myoepithelial cells
Cyto: 3D cell clusters surrounded by homogenous acellular BM
- biphasic cell population c large, clear myoepithelial cells and small, dark ductal cells
- naked nuclei
- proteinaceous spheres can look like adenoid cystic carcinoma
Px: locally aggressive low-grade tumor
Mammary Analogue Secretory Carcinoma (MASC)
Rare, recently described neoplasm that resembles secretory carcinoma of the breast and occurs in the parotid glands of older men
- previously recognized as acinic cell carcinoma or adenoca, NOS
Cyto: Dispersed / loosely cohesive cells in papillary or pseudopapillary arrangement c large polygonal cells c lots of vacuolated reddish cytoplasm and indistinct cell borders and bland round nuclei
- extracellular mucoid material common
Genes: ETV6-NTRK3 rearrangement
Px: similar to low-grade salivary gland tumors
Malignant Mixed Tumor
Can occur in 3 situations:
- Carcinoma ex pleomorphic adenoma
- metastasizing mixed tumor
- carcinosarcoma
Carcinoma ex PA is the MCC
- risk up to 1/10 for PAs present > 15 years
- may be able to tell clinically if mass is rapidly enlarging and painful
Metastasizing mixed tumor is a b9 PA that has met'd
- usually assoc c some type of surgery to a PA
- even though looks b9, this thing is usually lethal
Carcinosarcoma is rare
- should be able to recognize epithelial and mesenchymal cells
Myoepithelial carcinoma
Rare, can have inc cytologic atypia, necrosis, inc mits, infiltrative growth, 2/3 arise in PA's
Oncocytic carcinoma
can have variable pleomorphism, coarse chromatin
- hard to dx by cytolog alone
- ddx: oncocytoma, acinic cell carcinoma
Polymorphous low-grade adenocarcinoma (PLGA)
MCC malignant of minor salivary glands in children
- only occurs in minor salivary glands
Difficult dx to make on FNA; usually in minor salivary glands of older adults
- see cluster, tubules and cords of uniform cells c fine chromatin and variable architecture
- may also see hyaline globules (similar to adenoid cystic carcinoma), except nuclei are normochromatic (not hyperchromatic)
Likes perineural invasion
Salivary Duct Carcinoma
MC in older men; uncommon overall; clinically aggressive
- rsemble comedo ductal carcinoma of the breast
Cyto: Sheets and clusters of large polygonal epithelial cells c obvious malignant features such as large polygonal epithelial cells, irreg nuclear contours c prominent nucleoli
- necrotic background
IHC: AR and HER2 positive
Primary Small Cell Carcinoma
Rare malignant tumor c small undifferentiated cells, usually c some NE features
- is a dx of exclusion, as resembles small cell ca of the lung and cutaneous Merkel cell ca (must be r/o)
Cyto: virtually identical to small cell ca of lung, c loosely cohesive clusters of round to oval small cells c dark nuclei, no nucleoli, high NC, nuclear molding and freq mits in a cellular smear c necrosis
IHC: (+) CK20 [negative in small cell ca of lung, but + in Merkel cell ca]
Squamous cell carcinoma
Rare to have primary SCC of salivary gland, much more common to have mets from other site
- HG non-K SCC can look like other salivary gland ca's, esp MEC

LESA


Sialadenosis


PA
PA - trolls hair

Myoepithelioma: spindly, plasmacytoid, and epithelioid



Basal cell adenoma

Oncocytoma
Oncocytoma


Warthin tumor


Low-grade MEC

Acinic cell carcinoma

high-grade MEC

MEC

Adenoid cystic ca
MASC



Carcinoma ex PA
PLGA

Salivary duct carcinoma, AR and HER2 +


Small Cell Ca

SCC
References
1.
