Respiratory
Lung Embryology
Respiratory histology and anatomy
- Upper respiratory tract
- Lower respiratory tract
- Alveolar anatomy and histology
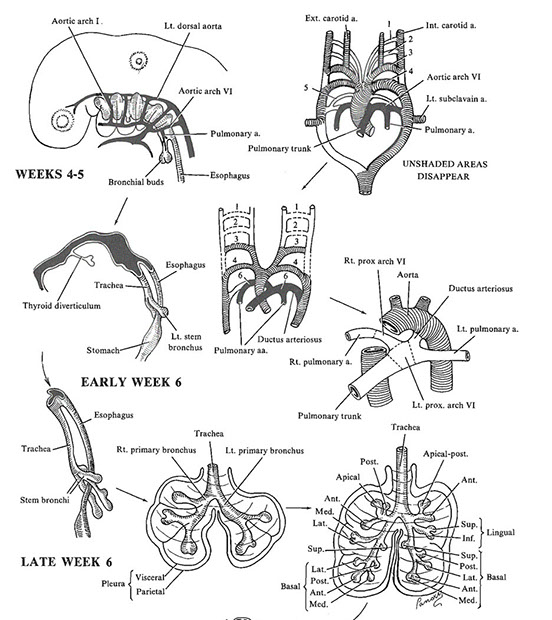
Lung Embryology
Arises from foregut endoderm as a ventral diverticulum that becomes trachea and larynx proximally and lungs and bronchi distally
- primary lung bud developed by 4 2/7 weeks post-fertilization
Postnatal histo
Bronchi are supported by cartilage plates which are larger proximally and have seromucinous glands; lined by stratified ciliated cells
- bronchioles do not have cartilaginous plates nor seromucinous glands; lined by single layer of stratified cells
Bronchus-Associated Lymphoid Tissue (BALT) can be seen in newborns and infants
5 developmental stages of lung development
1) Embryonic (3-4 wks to 6-8 WGA)
Milestone: Proximal airways
Lung made of primitive bronchial buds made of small simple tubules lined by thick layer epithelium within a bed of loose mesenchyme
2) Pseudoglandular (6-8 wks to 16 WGA)
Milestone: Distal (pre-acinar airways)
Progressive branching of bronchial buds giving rise to generations of airways
- forms larger proximal airways lined by stratified epithelium c goblet cells and smaller distal airways c simple epithelium
- cartilage starts to form around airways and major vessels
3) Canalicular (16 wk to 26-28 WGA)
Milestone: Acinus and primitive capillary network
Begins airspace development and capilarization of these primitive airspaces; tubules get increasingly branched and complex
4) Saccular (26-28 wks to 32-36 WGA)
Milestone: maturing alveolar-capillary interface
First see formation of secondary crests (ridges c double-layered capillary netwrk and protrude into airspaces
- mesenchyme becomes increasingly thin
5) Alveolar (36 wks to 2-4 years postnatal age)
Milestone: Increasing acquisition of alveoli
Amt of mesenchyme even more decreased to form thin intralceolar septa
- alveoli in mature back-to-back form lined by flat, mature epithelium
Respiratory Histology and Anatomy
Upper respiratory tract
Consists of nasal cavity, oral cavity, pharynx and larynx
- nasal cavity with squamous cells at nare entrance and pseudostratified ciliated cells in rest; oral cavity has just squames; vocal cords with squames
- upper pharynx is pseudostratified ciliated columnar, middle and lower pharynx with squames
Lower respiratory tract
Trachea - pseudostratified ciliated columnar cells supported by cartilage
Bronchi - same as trachea; bifurcates at carina
- have submucosal glands with cells that secrete mucuous or serous substance, Kulchitsky / enterochromaffin / argentaffin cells that secrete serotonin and calcitonin
Goblet cells - usually found with ciliated columnar cells, they may appear columnar with large vacuoles and eccentric nuclei
Bronchioles - functionally separated into terminal and respiratory bronchioles; has no supporting cartilage
- ciliated cells continue until respiratory bronchioles, at which point they become cuboidal (sans cilia)
Clara cells
Nonciliated, columnar c secretory granules
Secrete component of surfactant
Degrades toxins
Acts as reserve cells
Alveolar Anatomy and Histology
Type II pneumocytes
3% of alveolar surface
Secretes pulmonary surfactant (dipalmitoyl phosphatidylcholine)
- dec alveolar surface tension
- Lecithin:sphingomyelin ratio of >2.0 in amniotic fluid indicative of fetal indicative of fetal lung maturity
Cuboidal and clustered
- can also serve as precursor to type I cells
Prolierate during lung damage
Type I pneumocytes
97% of alveolar surface
squamous
- thin for optimal gas diffusion
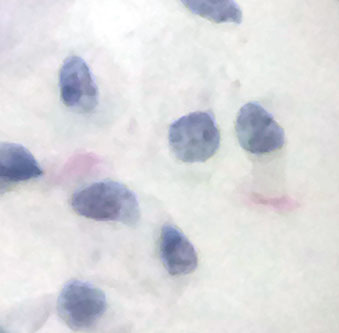
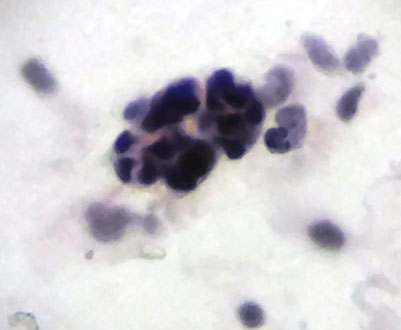
Macrophages
If found on slide, means that specimen must have come from deeper parts of respiratory tract, as they are usually found in alveoli
Round with fine cytoplasmic vacuoles, round eccentric nuclei, rarely have nucleoli
- multinucleated if reactive
- called "dust cells" if filled with anthracotic pigment
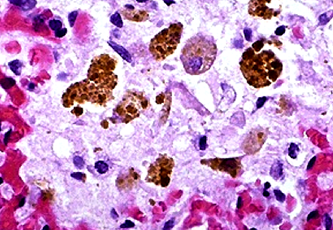
- "heart failure cells" are macrophages with ingested RBCs; can be highlighted with Prussian blue stain
- lipophages - macrophages with ingested lipids seen in newborns with pneumonia (inhaling milk)
1 Ciliated epithelium 2 Goblet cell 3 Gland 4 Cartilage 5 Smooth muscle cell 6 Clara cell 7 Capillary 8 Basal membrane 9 Surfactant
10 Type I pneumocyte 11 Alveolar septum 12 Type II pneumocyte
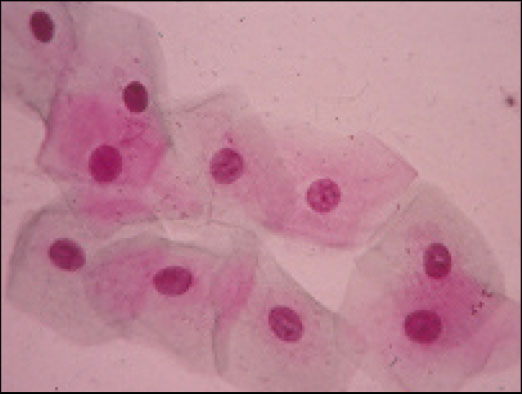
Squamous cells
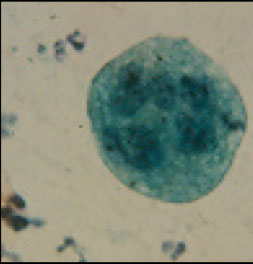


Macrophages
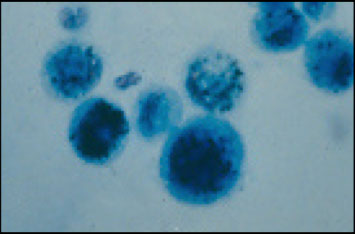
Dust cells (macros)
Lipophages
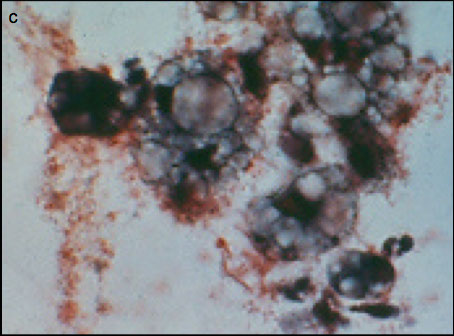
Heart failure cells (macros)
Ciliated columnar cells with red-eyelash cilia
Reserve cells
References
1. https://anatomytopics.wordpress.com/2008/12/08/8-the-anatomy-and-histology-of-the-trachea-and-lung-the-development-of-the-respiratory-tract/
2. http://www.embryology.ch/anglais/rrespiratory/phasen07.html
3. http://bmb.oxfordjournals.org/content/early/2011/07/01/bmb.ldr028/F2.expansion.html
4. http://discovery.lifemapsc.com/library/review-of-medical-embryology/chapter-59-development-of-the-lower-respiratory-system-the-bronchi-and-surrounding-structures
5. https://www.studyblue.com/notes/note/n/cellular-organells-/deck/3323208
