Head and Neck Cytology
General
Branchial Cleft (Lymphoepithelial) Cyst
Epidermal Inclusion Cyst
Oropharyngeal SCC
Sialadenosis
Adenoid Cystic Carcinoma (ACC)
Metastatic breast carcinoma to the neck
General
Indications for head and neck FNA:
- suspicious lumps and bumps
- first step in initial diagnosis of oropharyngeal and nasal cavity tumors
- mets to H&N LNs
- recurrent carcinoma after rad tx
Most childhood lesions are benign (90-95%)
In adults, 80% of non-thyroid neck masses are neoplastic / malignant
- 80% of primary malignancies found above clavicle
3 main types of cells in epidermis:
Squamous cells: These are flat cells in the outer part of the epidermis that are constantly shed as new ones form.
Basal cells: These cells are in the lower part of the epidermis, called the basal cell layer.
Melanocytes: These cells make the brown pigment called melanin, which gives the skin its tan or brown color. Melanin acts as the body’s natural sunscreen, protecting the deeper layers of the skin from some of the harmful effects of the sun.
Branchial Cleft Cyst
- aka Lymphoepithelial cyst
Classic lateral cyst
No sex predilection
May occur at any age, though more common in young adults
Usually occur along anterior border of sternocleidomastoid muscle
May present clinically as a firm, rapidly growing mass
FNA obtains turbid brown or yellow fluid
Cyst lined by squamous or glandular epithelium
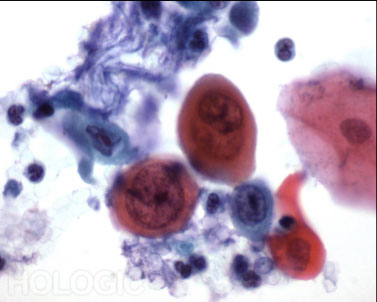
Cytologic features:
Anucleated and nucleated squamous cells
+/- reactive / degenerative atypia
+/- Glandular cells
Lymphocytes
Macrophages and debris
If inflamed, acute inflammation and granulation tissue may be seen
DDx: W.D. SCC and other neck cysts (ie. Thyroglossal duct cyst)


Thyroglossal Duct Cyst
Classic midline cyst(often near hyoid bone)
No sex predilection
Wide age range, but usually presents before age 20
Arise from embryologic remnants of thyroglossal duct
Cyst lined by thyroid tissue
Grossly aspirated fluid appears, may be clear, mucinous or “grungy”
Cytology:
Sparse cellularity
Macrophages and debris
+/- Respiratory columnar cells
Squamous cells may be seen
Thyroid tissue rarely sampled
DDX: Thyroid cyst
Any thyroid disease can occur in cyst!


Epidermal inclusion cyst
Most common cutaneous cyst
Occur in subcutaneous tissue, usually following trauma
May present anywhere on the body, but commonly seen on the face, neck or trunk
Mound shaped cyst with central punctum
Cyst filled with thick, cheesy keratinous debris, which has a characteristic foul odor
DDX: Dermoid cyst, Trichilemmal cyst (Pilar cyst)
Cytology:
Predominantly anucleated squames, though nucleated squames may also be present
Keratinous debris, occasional neutrophils and cholesterol crystals may be seen
If cyst ruptures, granulomas (aggregates of epithelioid histiocytes) and inflammatory atypia may occur
Cytologically similar to congenital Trichilemmal cysts and Dermoid cysts…Epidermoid cyst is also a general term
Trichilemmal (pilar cysts) derived from hair follicles occur in areas with hair (Scalp)
Dermoid cyst occur along embryonic line of closure
-Few nucleated squames may be present
-Smell bad (ICK!)


Abscess formation(suppurative inflammation)
May be caused by an inflammatory or infectious process
Tender, pink to deep red in color and warm to touch
Center of abscess is full of pus containing dead tissue, dead neutrophils and debris
Most are sent for microbiologic studies
Can have lots of actinomycotic colonies

Tszank Smear
Introduced by the Frenchman Arnault Tzanck, and has been used for many years in the diagnosis of bullous and vesicular dermatoses .
Samples are taken from a fresh vesicle
The vesicle is unroofed or the crust removed
The base is scraped with a scalpel or the edge of a spatula.
The material is transferred to a glass slide by touching the spatula to the glass slide gently.
Granulomatous disease
- Localized Nodular Inflammation
May be seen in numerous body sites including lymph nodes
Commonly occur in response to immunologic, idiopathic, neoplastic, infectious, and fungal processes
Lupus, Sarcoid, TB, Coccidiomycosis
May also be seen in certain malignancies
Squamous cell carcinoma, lymphomas (ie. HD and T-cell types) and certain Germ cell tumors
Cytology:
Aggregates of epithelioid histiocytes
+/- Multinucleated giant cells
Acute (suppurative) or chronic inflammation
Granulation tissue, macrophages, cell debris
+/- necrosis (caseating)
Sarcoid (non-caseating)

Pt c TB c mass on rt neck
Lipoma
Most common mesenchymal neoplasm
Slow growing and usually painless (can be painful)
Adults, typically 40s or 50s
F>M
Usually present as single, soft superficial masses (can be multiple)
Indistinguishable from normal body fat
Cytologically:
Lipocyte:
Large round cell
Optically clear, lipid droplet fills cytoplasm leaving thin rim of visible cytoplasm
Small round nucleus is pushed and flattened to the side of cell
Mature lipocytes occurring in tissue fragments with few single cells
Delicate inconspicuous capillaries
“Chicken wire” appearance
Grossly: oily material that beads up on air-dried slides and may dissolve during processing


Pilomatrixoma
- aka Calcifying Epithelioma of Malherbe
Relatively uncommon primary tumor of the hair follicle
Slow growing dermal or subcutaneous nodule
50% occur before age 20, but may be seen at any age
50% occur in Head and Neck region
A bluish skin discoloration is characteristic, but not always seen
Common source of diagnostic error
Triad of:
Ghost cells
Aggregates of degenerate, anucleate keratinized squamous cells
Basaloid cells
Tight clusters, sheets or singly
Small round cells, variably sized
Hyperchromatic to granular chromatin
May have small nucleoli
Increased N/C ratios
Foreign body giant cells (MNG)
Inflammatory cells, calcium granules, debris
occasional epithelioid histiocytes
DDX: SCC, Basal cell ca., Small cell ca.


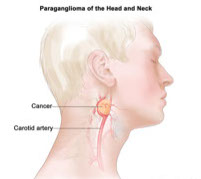
Paraganglioma
Most common site of extra-adrenal paraganglioma (within adrenal medulla “Pheochromcytoma”)
Present at angle of mandible / bifurcation of common carotid artery, as slow growing painless mass
Also associated with hepatic cirrhosis, Carney triad, MEN 2, VHL, and NF1
Rarely produces catecholamines
Mean age 40s , F>M
90% benign, 90 - 95% solitary
May invade locally or spread to lymph nodes or lung
Well defined cell nests of ovoid to spindled shaped chief cells with finely granular chromatin and abundant eosinophilic cytoplasm were surrounded by sustentacular cells, and embedded in a well vascularized stroma (Figure 6).
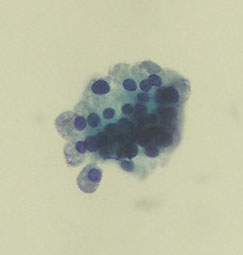
Cytology
Carcinoid-like or spindle cells
May be uniform to pleomorphic and bizarre
Nuclei are typically round to oval or spindle shaped
Salt and pepper to dense hyperchromatic chromatin
Intranuclear cytoplasmic invaginations may be seen
Ill-defined granular cytoplasm
Diff-Quik may show fine red neurosecretory granules
Cells arranged singly, in loose clusters with rosette formation and rounded aggregates of tumor cells (Zelballen)
Background typically bloody with varied cellularity
DDX: Medullary thyroid ca., Papillary thyroid ca, Sarcoma, Melanoma


Nerve Sheath Tumors
- Benign Schwannoma (neurilemmoma) and Neurofibroma
Schwannomas are more commonly aspirated than Neurofibromas
Difficult to distinguish cytologically
Diagnostic term commonly used “Nerve sheath tumor”
Slow growing, painless tumors
F=M
Benign schwannoma - deletion of chromosome 22 and NF2 inactivation
Neurofibromas – NF1, von Recklinghausen disease
Schwannoma
FNA may cause sharp radiating pain (“electric jolt”)
Composed of Schwann cells
Antoni A (ordered, cellular)
Antoni B (loose, myxoid)
Cytology:
Spindle cells with round to wavy nuclei
Bent, fishhook or comma shaped
Fine chromatin with inconspicuous nucleoli
+/- INCI (“kern-loche”: “Nuclear holes”)
Pale, fragile cytoplasm
Naked nuclei in the background
Fibrillar ground substance
Occur in loose aggregattes and nuclear palisades
Verocay bodies
Oropharyngeal SCC
Most common malignancy in Head and Neck region
Well differentiated to poorly differentiated, including basaloid types
Most are are moderately differentiated
25% HPV16 positive
Basaloid type often HPV16 positive
Favorable prognosis
FNA is commonly used to diagnose or exclude recurrent/ metastatic SCC in Head and Neck region
Risk factors for primary squamous cell carcinoma of the Head and Neck:
75%-Alcohol and tobacco abuse
2x more common in males
mid 50s to early 60s
Oral sex, open mouthed kissing
HPV16 positive
M>F
Avg. 58 yrs
AssocRisk factors for primary squamous cell carcinoma of the Head and Neck:
75%-Alcohol and tobacco abuse
2x more common in males
mid 50s to early 60s
Oral sex, open mouthed kissing
HPV16 positive
M>F
Avg. 58 yrs
c high risk HPV
Low risk strains: 6 and 11
High risk strains: 16, 18 33, 35, and 37
16 associated with SCC
18 associated with Adenoca
Risk factors for SCC of skin:
Ultraviolet rays from the sun or indoor tanning
May occur de novo
Pleomorphism
Anisonucleosis
Hyperchromatic to coarsened chromatin
Dense“waxy”cytolplasm with well-defined cell borders
Atypical parakaratosis
Cytoplasmic keratinization
Pearl formation
Necrosis
Keratininzing SCC commonly undergoes cystic degeneration including cystic metastasis
Elicits a foreign body granulomatous reaction and marked acute inflammation

Nasopharyngeal carcinoma aka. lymphoepithelioma
P.D. SCC with a lymphoid infiltrate
Associated with Ebstein-Barr virus
M>F
Peak incidence in teens and 50s
More common in certain parts of Asia, Southern China, Northern Africa, and Inuit populations in Alaska and Canada
Salt-cured fish possible risk factor
salt-preserved fish containing carcinogenic nitrosamines
Keratin, EMA, EBV, EBER; often p53, variable CEA, variable S100
Cytology: Large round, oval or spindle shaped cells Vescicular chromatin with prominent nucleoli Pale, fragile cytoplasm Numerous bare nuclei Syncytial –like arrangements Background of lymphocytes and occasional plasma cells
DDX: DLBCL, melanoma, Oropharyngeal nonkeratinizing carcinoma, Rhabdomyosarcoma

Merkel cell carcinoma
Uncommon neuroendocrine carcinoma of the skin
Head and Neck, appendages, buttocks
M>F
>65 years
>90% occur in Caucasians
Firm, painless, flesh colored to red-violet nodule
Risk factors
Sun exposure,chronic immunosuppression, Merkel cell polyoma virus
Monomorphic small round blue cells
Isolated, in small clusters and syncytial arrangements
Powdery to salt and pepper chromatin with minimal nuclear membrane irregularities
Inconspicuous nucleoli
Scant cytoplasm
IHC Positive: Low molecular weight keratin, CK20 (perinuclear dot like staining), EMA, neurofilament, neuron-specific enolase, CD56, Variable chromogranin, synaptophysin and CD117
IHC Negative: TTF1, CD45/LCA

Melanoma
Arises in melanocytes
Average age of diagnosis is 62, but it is not uncommon in individuals under 30
20% more common in Caucasians than African Americans
Risk factors
Exposure to UV light
Fair skin, freckling, light hair
Moles
Family history of melanoma
Xeroderma pigmentosum
Cellular smears
Dispersed single cells and loose clusters, prominent nuclear inclusions that can be confused with herpest
Commonly epithelioid and spindle shaped
Abundant cytoplasm, eccentric nuclei
Variable anisokaryosis and pleomorphism, binucleate and multinucleate cells
“DMIN”- Dual mirror image nuclei
Uniformly hyperchromatic, INCIs, prominent nucleoli
Melanin pigment
Tumor cells - intracytoplasmic
Macrophages
In background
Amelanotic pigment may not be seen
Main altered pathways include RAS-RAF-MEK-ERK, p16(INK4A)-CDK4-RB and ARF-p53 (APMIS 2007;115:1161)
20% of melanoma prone families have point mutation in CDKN2A locus at 9p21 which encodes p16(INK4a) and p14(ARF) (Br J Cancer 2008;99:364)
10% of cases may be familial due to CMM1 gene at 1p36
Microsatellite instability seen in pediatric melanoma (43%), adult melanoma (30%), nevi (9%, Am J Dermatopathol 2005;27:279)



Melanoma
Basal Cell Carcinoma
Most common form of skin cancer
Slow growing, rarely metastasizes
Occurs in sun exposed areas of the elderly, commonly in the head and neck area
If left untreated, it can grow into nearby areas and invade the bone or other tissues beneath the skin.
Presence as a nodule or ulcer (“rodent ulcer”)
DDX: Merkel cell, SCC
If not removed completely, basal cell carcinoma can recur (come back) in the same place on the skin. People who have had basal cell skin cancers are also more likely to get new ones in other places.
Small cells with scanty cyanophilic cytoplasm; indistinct cell borders
Small, hyperchromatic, oval, overlapping nuclei
Tight cell aggregates with sharp outlines
Peripheral palisading of nuclei
+/- stromal material
Kaposi's Sarcoma
This neoplasm is caused by human herpesvirus-8 and is derived from infected endothelial cells
It is an AIDS-defining illness and one of the commonest neoplasms seen in homosexual AIDS patients
Multiple blue/violet dermal nodules/plaques on the face, genitalia and lower extremities feet and legs
May be polypoid
Low cell yield; irregular tissue fragments of haphazardly arranged spindle cells
Elongated, blunt-ended, mildly irregular hyperchromatic nuclei with inconspicuous nucleoli
Poorly defined cytoplasm, which in some cases in the Giemsa stain is delineated by metachromatic stroma between the cells
Single spindle cells with bipolar or long and wispy cytoplasm
Hemosiderin-laden macrophages
+/- WBCs
Bloody background
IHC Positive:
CD31, CD34, Factor VIII related antigen, podoplanin (D2-40), thrombomodulin, latent nuclear antigen-1 of HHV-8
Molecular:
Diploid and clonal
HHV8 present in almost 100% of lesions (classic, HIV, or other types)


Embryonal Rhabdomyosarcoma
Most common primary Head and Neck tumor in children
Average age 6.5 years
Favorable prognosis as compared to Alveolar and Pleomorphic (adults) subtypes
Cytology
Triad of “small blue cells”, rhabdomyoblasts (spindle and strap cells), and myxoid matrix
Small blue cells are round with fine hyperchromatic chromatin, rare INCIs, and scant cytolplasm
Rhabdomyoblasts are spindle to strap shaped cells with similar nuclear features as SBCs with more abundant cytoplasm. Cross-striations are rarley seen
Myxoid stromal fragments appear metachromatic in Diff-Quik type stains
IHC stains
Vimentin+,Desmin+, Myogenin/MyoD1+
Molecular/Cytogenetics
No diagnostic translocation found to date
DDX: Other small blue cell tumors (ie. neuroblastoma, retinoblastoma)
Embryonal Rhabdomyosarcoma

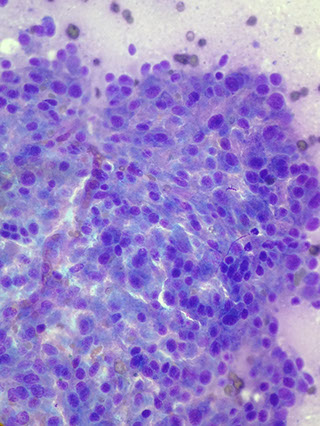
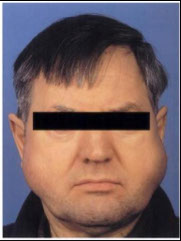
Sialadenosis
-Refers to nonneoplastic noninflammatory swelling in association with acinar hypertrophy and ductal atrophy. Usually bilateral parotid gland involvement
-Aspirates appear normal except acinar cells are significantly larger than normal and inflammatory cells tend to be absent.



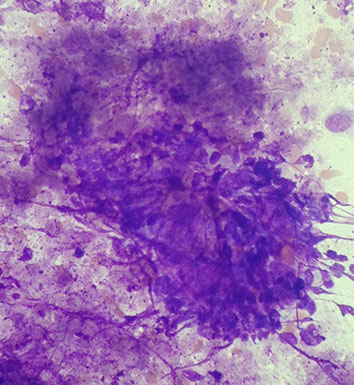
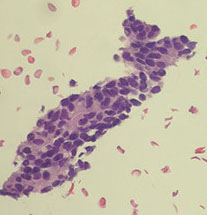
Adenoid Cystic Carcinoma (ACC)
Variably sized, often large , 3-D, acellular hyaline matrix globules and linear branching structures
Matrix is acellular with sharp borders (“cookie-cutter” like)
Basaloid cells
(Arrows show transparent hyaline globules on figure to left)



Metastatic breast carcinoma to the neck
FNA of neck node in older female with history of breast cancer
or currently has a breast mass, and no other lesions
Smear shows adenocarcinoma – Likely breast origin



MFH


RCC Mets
RCC mets
met prostate
