Intro to Gyn Cytology
Gynecologic Cytology - Cancer Spectrum
General Pap info
ThinPrep
Superficial cells
Intermediate cells
Parabasal cells
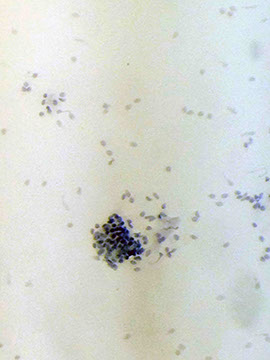
Lactobacilli
Glove powder crystals
Cocci bacteria
Anucleated squames
Sperm
Squamous pearls
Parakeratosis
Hyperkeratosis
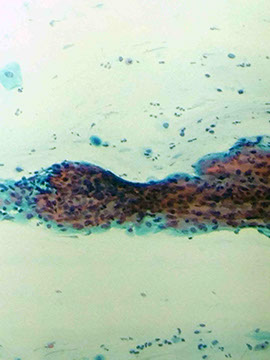
Lymphoid follicle
Lower Uterine Segment (LUS) cells
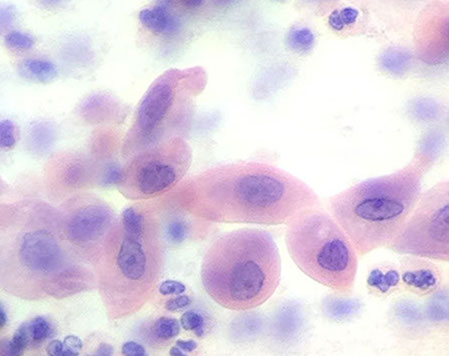
Squamous metaplasia
Tubal metaplasia
Dysplasia
ASCUS / ASC-H
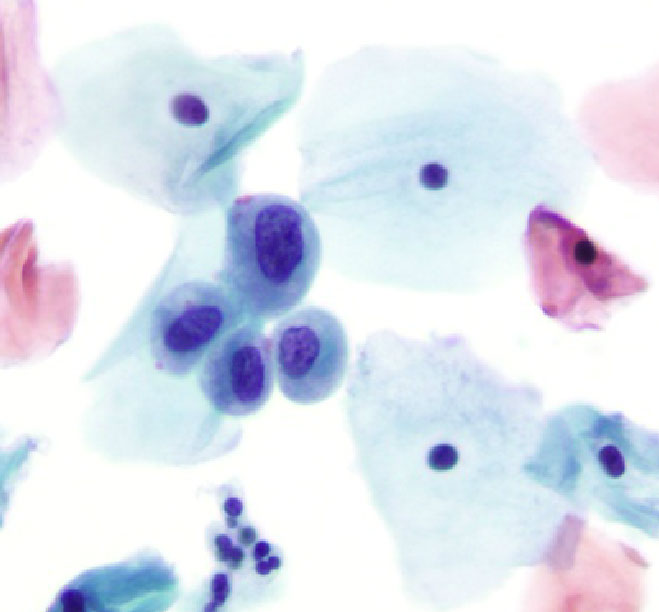
Carcinoma in Situ (CIS)
LSIL
HSIL
Squamous cell carcinoma
Glandular cells
Adenocarcinoma in situ (AOS)
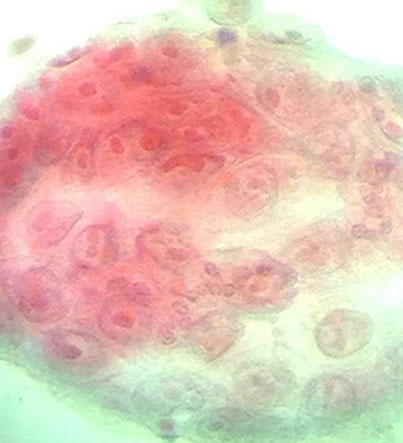
Endometrial adenocarcinoma
Endocervical adenocarcinoma
Clear cell carcinoma (of the vagina)
Small cell carcinoma

Culdocentesis / Ovarian Neoplasms
Overview / normal / reactive cells
Atypical cells
Differential diagnosis
Transformation zone
Endocervical cells
Endometrial cells
Gyn Hormonal Patterns
Inflammation / Histiocystes / Repair / Atrophy / Radiation
Background - Bugs - Candida, Schistosoma, Trichomonas, Leptothrix, Herpes simplex, Chlamydia, ActinomycesGardnerella vaginalis, HPV, Granuloma inguinale, Gonorrhea
General Pap info
According to Clinical and Laboratory Standards Institute:
- schedule Pap 2 weeks after 1st day of last menstrual period
- Do not put lube on speculum (water can be used instead)
- Excess mucus can be gently removed
- Get sample before using any acetic acid or Lugol iodine
- Should have transitional zone cells (both ectocervix and endocervix) [not required for a "satisfactory" smear, but is a quality indicator] -- in order to report transitional zone must hav 10 good-looking endocervical or squamous metaplstic cells present
- ANY abnormal cells makes the specimen an adequate specimen
- colposcopy performed with ASCUS and abone
Per 2012 guidelines by American Society for Colposcopy and Cervical Pathology Consensus :
- start screening at 21 yo regardless of whether pts has had sex or not
-- pts younger than 21 yo do not get tested regardless of age of sexual onset
- Pts 21-29 yo get tested c Pap test only at 3-yr intervals (do NOT get tested for HPV)
- Pts 30-64 get Pap tested at 3-yr interval (Pap only) or 5-yr interval (Pap and HPV)
- testing can be stopped if pt gets either 3 consecutive neg Paps or 2 consecutive neg HPV with Pap
- can also stop testing if pt has no hx of abnormal paps and gets a hysterectomy for a b9 condition
- pt must continue to get screened for 20 yrs after hysterectomy for a malignant condition
- repeat cytology performed at 2-4 mo if inadequate specimen and neg- or unknown-HPV test resuls
When evaluating sample, judge "satisfactory" as:
- 5,000 squamous cells on liquid-based smears, 8-12,000 on conventional smears
- less than 75% of obscuring elements (inflammation or drying artifact)
*** 5 alive !!!! ***
- if Pap is unsatisfactory, woman should get another Pap test done in 2-4 mo
- if woman has 2 unsatisfactory Paps consecutively should get a colposcopy
-- colposcopy also done in women who are HPV 16 or 18 pos
- women c negative cytology test and pos HPV 16, the risk of HSIL or worse is 18-20%
Max # of slides cytotech can read in 24 hrs is 100
If slide is previewed first with digital automated system and then the whole slide is manually reviewed, counts as having reviewed 1.5 slides per CLIA rules and regulations
CLIA '88
Cytotechs screen all gyn specimens and only abnormal smears (reactive/repair and above abnormalities)
- pathologists review all non-gyn specimens (normal or not)
-- pathologists must review 10% of paps cytotechs call normal
- all HSIL are investigated, with review of the prev 5 yrs before diagnosis
- max number of slides for cytotechs: 100 slides in 8-hour day
Cytology gyn and non-gyn slides must be retained for 5-yrs
- FNA slides must be retained for 10 years
- requisitions for tests retained for 2 years
- pathology reports retained for 10 years
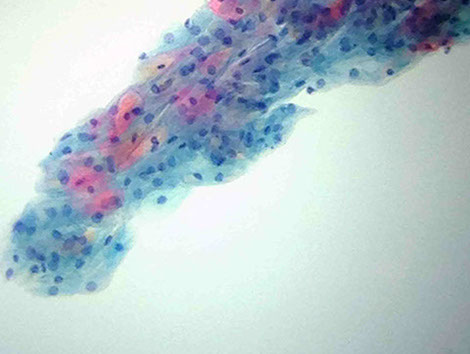
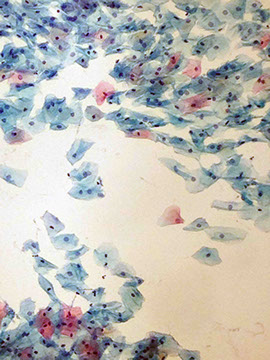
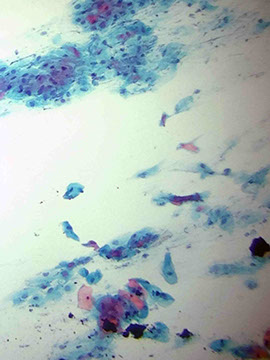
Group of intermediate cells
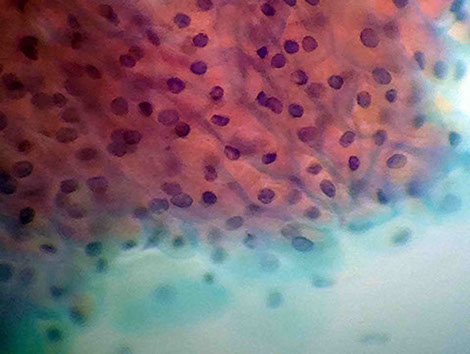
Red cytoplasm clustering artifact of intermed cells
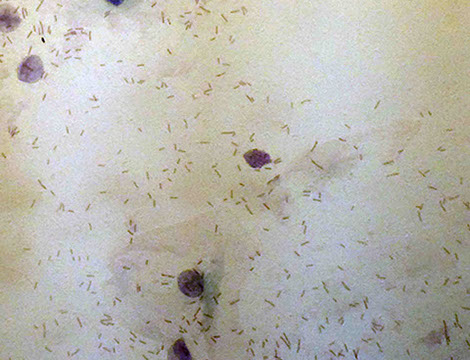
Cytolysis with doderlein bacteria
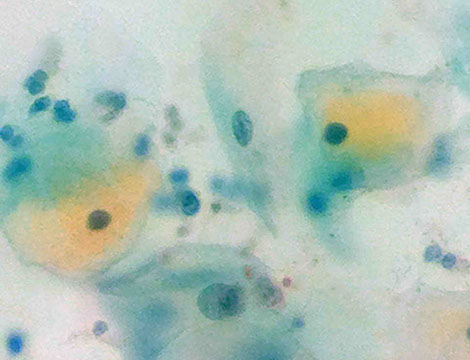
Glycogenated intermediate cells
Intermediate cell (Thin prep)
1 - 5
<
>
ThinPrep!!!
ThinPrep uses methanol to collect cells (better cell preservation)
3 phases:
1 - Dispersion
- cells stirred in their collection receptacle to mix em up
2 - Cell Collection
- suck up some cells into a cylinder from the collection receptacle
3 - Cell Transfer
- cylinder is inverted and presses up to a slide and blown on from behind
Cells are more uniformly distributed (not smeared)
Proportionately smaller due to wet fixation
- but has enhanced cytoplasmic and nuclear detail
- may have variable nuclear staining...
Cells round up in solution (?)
Single cells more prominent with enhanced nuclear detail
Chromatin pattern is variable, making morphological detail more important
Background is rarely obscured - which can be a bad thing if looking for a specific disease
- RBCs look like little ghost-like groups of balls
Must have systematic approach for screening a pap test, at a good pace that overlaps screening fields


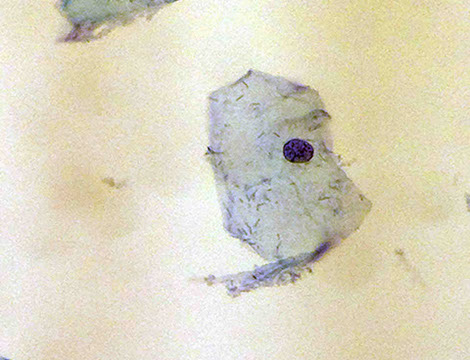
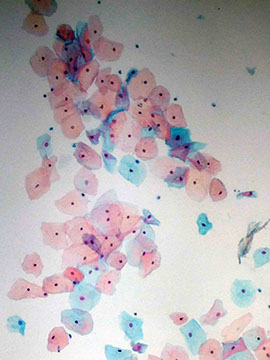
Superficial cells (above) from superficial squamous epithelium are thin, angular (pointy) with pale pinkish (eosinophilic) cytoplasm and a tiny black dot of a nucleus (the nucleus is pyknotic b/c the cell is no longer producing proteins and is in fact dying and being shed)
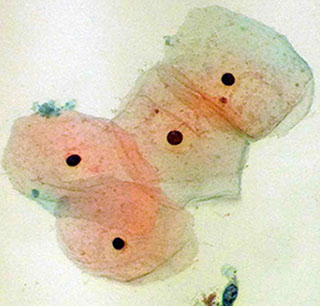
Intermediate cells aound beneath the superficial cells and have similar overall cell shape, but the nucleus is less eosinophilic, ranging om blue to light green and the nucleus is larger and vesicular (active, granular) indicating that it is still producing p
- these cells tend to cluster more than the superficial cells (which can produce the illusion or artifact of red/orange cytoplasm) and can have more wrinkles in cytoplasm and more variety in their shape (slide 2, above)
- Intermediates can undergo cytolosis due to the doderlein bacilli (which metabolize glycogen and produce acidic environment [pH 4.5] to keep other bugs [trichomonas] at bay), which is seen as stripped nuclei (slide 3, above)
- can be in neonates 2/2 blood from mama
- yellow appearance of cells due to glycogen stained by bismark brown; seen later in menstrual cycle and during pregnancy (slide 4, above)
Parabasal cells are the deepest of the squamous epithelium and are the most active cells, which is why they have the largest N:C ratio, with basophilic cytoplasm and nucleus with visible nucleolus (more eosinophilic) and some dark chromocenters within chromatin network of the nucleus
- may be seen in neonates 2/2 blood from mama




Lactobacilli
aka Doderlein's bacilli
MC organism seen, is a normal part of vaginal flora
- non-encapsulated rod-shaped bacteria that use glycogen present in glycogen-rich cells which causes cytolysis
Glycogen fermentation causes lactic acid production which keeps the vagina at a normal pH (of around 4.5)
- intermediate cells have the most glycogen (not so much in superficial or basal cells)
-- thus are rarely present b4 onset of puberty or after menopause
Lactobacilli

Glove powder crystals may be present, which stain
clear/purple. and have acellular, refractile look and may significantly
distort the smear
Anucleated squames (above) are ghostly cells with pink-orange-yellow motley crew
- may be contamination from vulva or a keratinizing condition (like leukoplakia or chronic irritation), and should be reported
-- can also be seen in elderly and in 3rd trimester pregnancy
Sperm may be on smear,
no one knows how they get there
- must be able to differentiate from
fungi,and tail is not always obvious
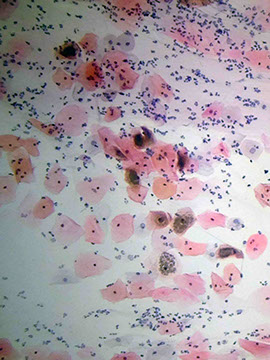
Cocci bacteria may appear as a fuzzy miasma that obscures the smear, which can look like a bunch of little balls if you stare for long enough
- usually assoc c infx
Squamous pearls come from scraping off clumps of squames that group together at the bottom of pits and seem to move in corkscrew fashion when moving up and down with fine focus
- usually mean that some other process, such as high-grade HPV, superficial hyperkeratosis, or squamous metaplasia going on
- can be harbinger of squamous carcinoma of the cervix, but can also be found in atrophic vaginitis and radiation-related changes







Parakeratosis

Parakeratosis
Keratinized cells with orange cytoplasm and elongated pyknotic nuclei
- benign reactive change usually assoc c chronic irritation
Hyperkeratosis
Anucleated mature, keratinized squames which are usually isolated or found in plaques
Hyperkeratosis

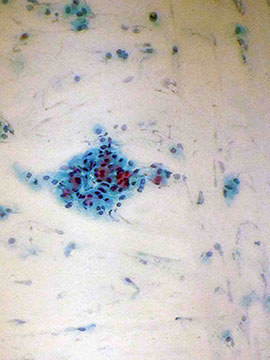
Follucular cervicitis

Lymphoid follicle
Group containing mostly lymphocytes of the small and sometimes large variety; can see tangible body macrophages in there sometime too
- tangible body macrophages are a clue for chronic folicular cervicitis
Follicular cervicitis
tangle of small blue cells c high NC ratios
- admixed histiocytes and dendritic cells c pale nuclei
- may be assoc c Chlyamydia trachomatis
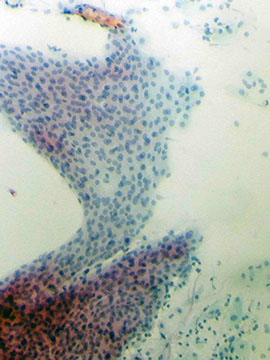
Lower Uterine Segment (LUS) cells
Found in groups c roun, uniform nuclei c evenly distibuted chromatin and nucleoli
Direct sampling so well preserved
frags of 2d shapes
can see gland opening and tubular arrangements
- oval to elongated nuclei c high N:C ratios
common after bx
- can look 3D if a piece gets rolled over onto itself
LUS cells

Transformation zone
Squamocolumnar junction that is at risk for ca!!
- is assessed by presence of endocervical cells
Goes way up into canal in older women
Reserve cell hyperplasia c prolif of basal cells, can go to either squames or glandular cells
- first get immaure hyperplasia then more mature hyperplasia
Endocervical cells
Line the endocervical canal, lets you know the transformation zone has been sampled
- uniform secretory or ciliated active columnar cells in HONEYCOMB or PICKET FENCE formation
-- thus will have more open, vesicular nuclei than squames (except from the lowest epithelial levels)
- small, smooth nuclei c vesicular, evenly distributed chromatin +/- nucleoli
Can resemble para-/basal epithelial cells
Cytoplasm is foamy and delicate (compared to heavier squame cytoplasm); usually clear or light blue/pink
Oriented horizontal and perpendicular to BM in 1-2 layers (squames are horizontal and stack in many flat layers)
- polarity of the cells helps to distinguish from other cell types
- endocervical cells overstain when superimposed on mucus or other cells
Cells can look big and malignant when reactive, esp in pregnancy (the Arias-Stella reaction)
Tubular metaplasia - can see cilia or terminal bars





Endometrial Cells

Exodus

Small columnar cells that line the corpus (body) of the uterus
Shed during menses with fragments of underlying endometrial stroma (CT); seen up until day 12 of menstrual cycle (in first 1/2 of cycle), when cytobrush used, with IUD present, when a lesion is present
Typically see a "double contour," with an outer layer of glandular cells surrounding an inner layer of condensed stromal cells
- vacuolated cytoplasm (?)
-- suspicious in post-menopausal women, and after day 10 of menstrual cycle
- also see blood, PMNs, and histiocytes
- are smaller (more shrunken), darker (more pyknotic), and have less organization than endocervical cells (qualities which are intensified as they travel down the endocervical canal and degenerate)
Tend to form tightly (sardine) packed, 3D balls with little intervening cytoplasm
- may see Hyperchromatic Crowded Groups (HCGs)
-- spontaneously shed endometrial cells in 1st 12 days of cycle have nuclei with irregular contours and form groups with scant cytoplasm
Exodus pattern (days 6-10): tightly packed group of endometrial cells that is darker on the inside and ligher on the outside (dual population: stomal cells on inside, endometrial cells on outside); shape can be variable
- histiocytes are more often single celled loners than in groups (but some have thought they both may have similar origins)
Stromal cells are similar to both endometrial cells and histiocytes, but do not have glandular nor foamy cytoplasms (respectively)
Should be reported in women >45 yo b/c of small inc risk of cancer! (do not need to be reported in chicks under 45 yo)
- since finding endometrial cells in older/post-menopausal women on Pap has inc risk of underlying enocervical carcinoma (1/20) or hyperplasia (1/9), finding endometrial cells in these pts will result in sampling of the endometrium and endocervical curettage




Gyn Hormonal Patterns
Estrogen level in blood has direct effect on the degree of squamous maturation, which can be accurately deduced based on the degree of squamous maturation
- effect can also be brought on by different hormones (prog, androgens, roids, ant pit hormones, etc)
- this judgement is based on a general Gestault of the cells present
Procedure used to be done by scraping cells off wall of vagina, not really used anymore
- cervical cells pretty inaccurate for this test; and cells around the cervical os generally do not respond to hormones
Can perform a count of 20-30 cells to get a more precise percentage if it is asked
May get interference from inflam, mucus, or metaplasia
Cannot comment on Maturation Index (MI) during a cervicitis or if anucleated squames are found
Grading system for estrogen effect (not really used anymore [?], but FYI):
(Abbrev. for MI is: parabasals/intermediates/superficial [P/I/S])
MARKED - 80% + superficial cells
HIGH - 50-80% superficial cells balance intermediate cells (0/40/60)
MODERATE TO HIGH - 30-50% superficial cells balance
intermediate (0/60/40)
MODERATE - Majority of cells intermediate, 10-30% superficial
(0/80/20 - 0/90/10)
SLIGHT TO MODERATE - Majority of cells intermediate, less than 10%
superficial (0/95/5)
- estrogen levels in this range will cause very few superficial cells to be
shed in the test, an effect that is common for this range; and there is
usually stripped nuclei, cytoplasmic fragments and a chopped up smear
pattern
SLIGHT - 100% intermediate cells (0/100/0)
VERY SLIGHT - Mixed intermediate parabasal and basal cells
ATROPHY (no estrogen effect) - parabasal and basal cells (100/0/0)
- occurs naturally post-menopause; intermediate cells and an occasional
intermed or superficial cell can be there
Maturation Index (MI) in smear patters are altered by infection and
erosion in the perimenopausal or postpartum periods
- is considered unsatifactory for eval of estrogen levels bc cell changes
not caused by estrogen
- used to be done by counting 300 cells
Menstrual cycle changes
Day 1-5 (Menses): Endometrials shedding most, shedding out single
cells, loss of cohesiveness, a little kidney-shaped, no mucin,
background is dirtier
- Onset menses: 0/80/20 --> 0/90/10, cells a little folded, some
bacterium present
Day 6-10 (Proliferative Phase): Endometrial glands forming again,
stroma in center, nuclei on inside, has some organization
Middle follicular phase: some estrogen starts to show up, see some
doderlein bacteria, fewer neutrophils
- day 12 is the peak of histiocyte activity
Late follicular phase: more estrogen, cleaner, less bacteria, most cells
superficial
Day 14 (ovulation): 0/60/40, peaks at 0/40/60, then waves up and down
a little bit, and comes down during proliferative phase to 0/80/20, has
cleaner background and inc Estrogen
Air-dried cells look faded and cellular detail is lost
During pregnancy there is little estrogen effect and you will see special intermediate cell, the navicular cell, that has yellow glycogen and its nucleus pushed out to the side
- MI during pregnancy --> 0/95/5 (majority intermediate)
- if right shifted during preg (-/-/++), must consider threatened abortion
- if anucleated squames seen, think Rupture of Membranes
- Parabasal cells / atrophic pattern in pregnancy, or a left shift (++/-/-) could possibly mean death of fetus; placenta uses fetal adrenal hormones as building blocks for ...???
Postpartum picture - similar to postmenopausal atrophy, but the cells appear better preserved and there is not as much air drying
- both will be inflammatory due to thin atrophic epithelium which is more susceptible to infx
- 6 wk's postpartum --> 100/0/0
- cytolysis can also be seen postpartum
May seen estrogen effect in newborns due to maternal hormone stimulation
Early/premature menopause can be assoc c 100/0/0 (sheets of parabasals in clean background; also seen in young children) or 0/100/0
- just don't expect estrogen effects in postmenopausal pt (unless taking hormones or due to pathologic tumor stimulation)
In late menopause, can see sheets of or small groups of parabasals
- cells appear flattened or pulled out and seem to merge seemlessly into larger clumps of cells
Rolled and folded edges are typical of atrophy and some cells have the tendency to spray out in flat squamous projections, but they don't curl up into glandular clusters
- will often see blood in smears with atrophy b/c the atrophic woman is thin and has poor protection against the procedure
Atrophic smears and primary amenorrhea (left-shifted) may appear metaplastic
- if hyperchromatic (dark) parabasal cells seen and you're unsure of malignancy, Estrogen should be given to the patient for 7 days and the test repeated to see if the cells have benignly matured to epithelial cells or if they have grown to big ugly hulkish metaplastic cells
-- Decidual cells mimic mildly dysplastic cells
--- dysplasatic cells are more organized than decidual cells
--- decidual cells have prominent nucleoli and ample cytoplasm (dec N:C) and only 1 single nucleoli (vs repair); and are more often seen postpartum (syncytiotrophoblasts can look like MNGHs)
Will often see inflammation bc they are more susceptible to infx
Repair has multiple nucleoli
Neonates under placental hormonal influence close to birth, then become atrophic after influence wears off
Anucleated squames can more frequently be seen in elderly pts and in 3rd trimester pregnancy



High estrogen effect
Moderate estrogen effect
High-marked estrogen effect
Moderate estrogen effect
Slight to moderate estrogen effect
slight to moderate estrogen effect with lots of doderlein bacteria eating glycogen
Slight estrogen effect c lots of doderlein bacteria eating glycogen
Atrophy
Atrophy
Atrophy (air-dried)
Early-phase of post-partum, lots of parabassals
Estogen levels returning to normal post-partum
Mild estrogen effect 6 months post-partum
Post-partum
Navicular cells in pregnancy
Pregnancy
<
>
5 - 16

Menstrual cycle progression (from Wikipedia)
Inflammation/ Histiocytes / Repair/ Atrophy/ Radiation
Inflammation
Is usually caused by bugs in gyn cytology, but can also be seen in pregnancy, menses, dysplasia or carcinoma
Cellular characteristics:
- Reactive (or active) nuclei and prominent nucleoli
- Amphophilic staining cells
- Empty or "salt and pepper" chromatin pattern
- Pleomorphism and bizarre cell shapes
- Dyskeratosis and pseudo-parakeratosis
- Perinuclear halos
- Karyorrhexis (chromatin pushed to border of nucleus and broken up; the stage before karyolysis) and pyknosis
- Metaplasia and/or mild dysplasia
- cytoplasmic vacuolization
"School of fish" are streaming cells with prominent nucleoli
Nuclear enlargement not enough to dx ASCUS

Histiocytes
Common in gyn cytology
Delicate pleomorphic cell c lacy, vacuolated cytoplasm
- cytoplasm stains anywhere from blue to red-/gray (amphophilic) and is very scant, or thin-appearing
Are constantly changing shape and can have a wide range of size
Nuclei very active with multiple chromocenters/nucleoli
Tend to be loner cells and form irregular aggregates rather than the geometric formations of endocervical or endometrial cells
Giant multinucleated histiocytes have many small oval nuclei and the regular amphophilic cytoplasm
- may closely resemble clusters of endometrial cells
-- different because GMNHs have round cytoplasmic border binding the nuclei together, as they are just one cell; another thing to look for is that the nuclei usually cluster together at one end of the cell
- endometrial cells also have less cytoplasm and generally lack the smooth border of GMNHs

Repair
Replacement of dead or damaged cells by new healthy cells from one of these processes:
- Inflam
- Radiation
- Post hysterectomy
- Recent cauterization or biopsy
Characteristics:
Low to moderately cellular smear
- cohesive flat sheets of cells which are presumably endocervicals (can sometimes be isolated cells;
- cyanophilic or sometimes vacuolated cytoplasm (cells still have cytoplasmic borders and should be able to walk around cytoplasm)
- background normal endocervical cells and moderate inflam
- Uniformly finely granular chromatin or less commonly coarsely granular
- Prominent eosinophilic macronucleoli; either single or multiple
- variable nuclear size (moderate), minimally enlarged (~2x normal intermed cell nucleus), large irregular nucleolus and possible bi- / multinucleation, but smooth nuclear membranes surrounded by abundant, flowing (pulled taffy) cytoplasm; thus normal N:C ratio
- can see occasional mitotic figures and WBCs engulfed (emperipolesis?)
Vs carcinoma, repair stays in well-polarized sheets (relatively shallow sheets, carcinoma is deeper) and can have enlarged nuclei but they stay smooth; nucleoli can be there also, but aren't in every nucleus
- chromatin pattern in carcinoma is more prominent and disordered



Atrophy
Epithelium starts to receive less and less estrogen from early 40's to mid 50's
- When E stops completely, cells wont mature beyond parabasal stage
-- Thus smears composed of parabasal cells are called "atrophic"
Parabasal cells can be in sheets or singly
"Blue blobs" may be found in atrophic smears
- may be degenerated parabasal cells' bare nuclei, or a dense mucus ball
-- benign finding; bare nuclei less likely to be seen on ThinPrep (b/c smearing artifact not there)
Wide-spread MIs may indicate that a post-menopausal patient has been receiving exogenous E
Nuclear enlargement is assoc c atrophy
Since the epithelium is thinner, it is more susceptible to infx, and it's not uncommon to see inflam
May see parakeratotic cells, which look like mini-squames
- may be malignant!
- may see Hyperchromatic Crowded Groups (HCGs)
Atrophic vaginalis: clumped cellular debris
Atrophy c blue blob



Radiation
Many of the changes in radiation can be suggestive of malignancy, and the changes can last for years
Tumor cells affected can appear extremely bizarre, but these cells provide no reliable clue for persistent cancer bc they are no longer able to divide / reproduce
- only ca cells that are unaffected can provide evidence of ca persistence
Thus, diagnostic tumor cells after radiation treatment must be free of radiation effect
Characteristics:
- cytoplasmic vacuolization (mostly a parabasal change)
- increased cell size (big nucleus and lots of cytoplasm) and pleomorphism, but normal N:C ratio
- bizarre cells (elongated)
- prominent nucleoli - reparative change
- multinucleation and reparative wrinkling
- two-toned cytoplasm
- nuclear vacuolation with finely granular chromatin
- network of mucus in background
- syncytial grouping
- should not see hyperchromasia
Irregular chromatin detail, hyperchromasia and inc N:C ratio are NOT radiation effects
Radiation effects can be divided into 4 eras:
(1) Acute: 1-6 months - See nuclear/ cytoplasmic vacuolization, huge nuclear enlargement, 2-toned cytoplasm, neutrophil phagocytosis, spider-like projections, inflam background, nuclear membrane of malignant cells are broken up
- do not comment on malignant cells (or HPV) during this time period
(2) Intermediate: 6-12 months - start to see reparative changes, look for MNGCs, can start to comment on malig cells (need to be ca free for 1 month)
- watch out for persistent cancersl have keratin (yellow) production
(3) Chronic: 1-5 years - Repair still taking place, whispy cytoplasm
(4) Late: >5 years: still see vacuoles
Are able to classify host response:
- Good response - MNGCs, background trying to clean up, left-shifted squames
- Poor response - also lots of inflam, but mostly eos and PMNs, no MNGCs, background doesn't clean up
Chemotx will make chromatin pattern smudgy and dysplastic-looking
- can look like HPV, can see cytoplasmic vacuolization and PMN phagocytosis



Background - bugs

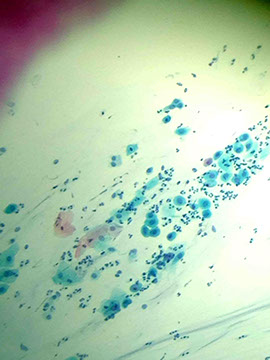
Candida spp
Common fungus seen in paps
Esp common in pregnant women, where it presents as irritation with thick cheesy exudates
- important to identify bc may cause infection in newborn
Micro: appear straw colored or a faintly amphophilic (blue or pink) with thin ruler-like hyphae which are segmented
- aspergillus may be confused with candida, but it has 45º angle branching
- Candida galbrata has only spores
Piling / clumping of squamous epithelial cells on low power may be the only clue for candida; a clue that tells you, "Hey, look at me on high power!!"; called the "shish-kebob" on low power
With candida the cells stick together like a Hawaiian lay(?), and you may see nuclear cavitation and folding of the cytoplasmic membrane
- can see engulfed WBCs
Sperm may also mimic candida, but they have a black and white head, whereas yeast spores are refractile capsules all around
Mucus can also mimic Candida

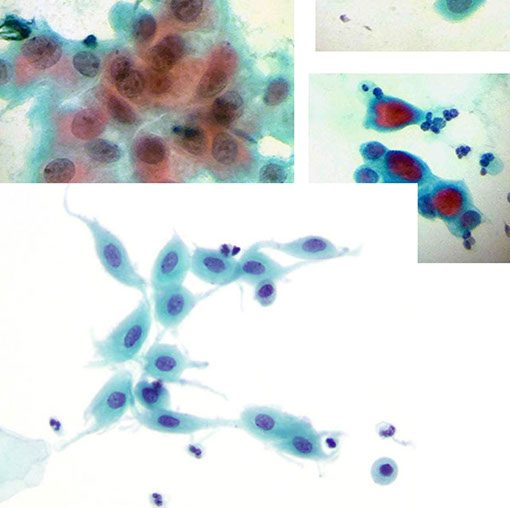
Trichomonas
Protozoan that raises the vaginal pH
- assoc c burning, itching, and
malodorous vaginal discharge
- most of the intermediate (most cells in general) will tend to stain more eosinophilic rather than their usual basophilia
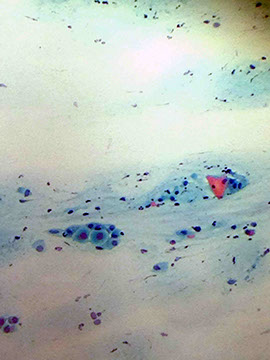
Micro: small, pear-shaped buggers with faint nucleus in the center (the "eye" of trich) that stains blue-green with a fuzzy appearance (unclear cytoplasmic borders) and variable amount of red cytoplasmic granules
- flagella usually is not observable
- depending on exact stain and pt response, may see inflam, metaplasia, bleeding, inc estrogen-like effect (pseudo-eosinophilia [intermediate cells can look reddish], active nuclei and degeneration
- usually accompanied by cocci, but can be seen with doderlein bacteria
Important features that may clue you in to Trich:
- watery background ("Trich trails" or snail trails)
- nuclear enlargement and perinuclear halos
- perinuclear and cytoplasmic cavitation
- "Trich parties" where numerous Trich's stick onto the outer surface of
squamous cells
- two-toned cytoplasm
- neutrophil "poly" balls
Tx: Metronidazole for pt and their partner(s)
Leptothrix also occurs with trichomonas
- looks like wavy, COOKED spaghetti smeared across the slide which does not branch and is thinner than candida; doderlein bacteria look like stiff, UNcooked spaghetti
-- Can see trich w/o leptotrix, but almost never see leptotrix w/o trich
Candida can also appear with trich
Trich trails
Schistosoma (no pictures)
Must always look in center bc you need to differentiate from a vegetable cell (who's center is much more refractile)
Pollen has refractile wall and is usually superimposed on slide and not on the same level as epithelial cells



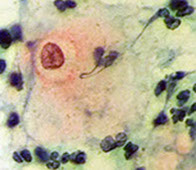


Herpes Simplex
Rarer than Candida
May affect squamous or glandular cells
The virus penetrates the nucleus and forms an intranuclear inclusion surrounded by a halo or cleared space, making the nuclei appear lobulated and multinucleated
- stages: the nuclei appear very active with prominent nucleoli, then the nuclei are glassy or empty and often multinucleated
- nuclei may appear glassy before the inclusion lobules form
Multinucleated cells mold together; the center is usually more opaque
- ground glass appearance is usually primary herpes infection; whereas nuclear inclusions are found in recurrent herpes infx (Cowdry type A bodies??)
-- Caveat! MUST be careful because atrophic background may give multinucleated, ground glass appearance as well
--- Make sure that nuclei are molding together and not just simply overlapping and nucleoli should be more angular than round
4 M’s = multinucleation, nuclear molding, margination of the chromatin, and “mulberry shaped”.
Plus large eosinophilic intranuclear inculsions.
CMV may have nuclear inclusions, but it is not multinucleated like herpes
Carpet Beetle
International pest, Could be 2/2 cotton in tamponds

Chlamydia spp
includes C psittaci and C trachomatis; which differ in life cycles (?)
- bc of life cycle classified in separate order than bacteria (lives in cytoplasm, not nuclear [like herpes]), though are very similar to gram-negative bacteria with coccoid appearance, anaerobic existence and rigid cell walls
Now reaching epidemic levels, this bug is assoc c multiple genital diseases and has properties of both bacteria and viruses (are similar to viruses bc they are energy parasites that are strictly intracellular)
Micro: Cause nuclei to become slightly enlarged, hyperchromatic and no nucleoli
- the cytoplasm is dense, cyanophilic, finely granular with sharp cytoplasmic borders
- endocervical cells and squamous metaplastic cells are usually affected
- are diffusely scattered throughout the cytoplasm with eosinophilic/cyanophilic coccoid structures, which can be separated by membrane-bound clear zones

Actinomyces
Actinomyces

Actinomyces
Lootks like dark blue gobs of stuff on the slide with filamentous excrescences at high mag
- can look like lube, but is more refractile
- assoc c IUD use
Entamoeba gingivalis
Assoc c IUD use
Entamoeba gingivalis

Gardnerella vaginalis
Causes bacterial vaginosis (BV), where pt has thin, milky discharge with a fishy odor
Micro: The clue is in the clue cells (epithelial cells covered with small adherent bacilli which appear granular);
- also see a few pus cells, lack of lactobacilli, background of small rods

Granuloma inguinale - macrophages c doderlein bodies or cocobacilli
vs
Gonorrhea - diplococci found in neutrophils
HPV
Perinuclear cavitation, hyperchromatic nucleoli, binucleation, thick refractile and sometimes orangeophilic cytoplasm (koilocytes)
- presence of koilocytes automatically qualifies as LSIL
Prefers to infect cells at the transformation zone
HPV is circular double-stranded DNA virus
- HPV 16 is MC strand found in cervical cancer (up to 60%), others carcinogenic strands are 18 (15%),
-- HPV 6 and 11 are low-risk strands
Cervical cancer caused by E6 binding p53 and E7 binding pRB
- L1 is a viral capsid and is the principal component of HPV vaccines
Adenocarcinoma assoc c HPV 18
- squamous lesions assoc c HPV type 16
50-60% of infected women have circulating HPV ab's
Guardasil is the HPV vaccine approved for females ages 9-26 containing HPV epitopes 6, 11, 16, 18 given by injection over a 6-mo period
- does not work if you're already infected by the virus
- Guardasil and Cervarix made of empyu protein shells called virus-like particles that are made of major HPV capsid protein L1
- are not infectious bx do not have genetic material
Gynecologic Cytology - Cancer Spectrum
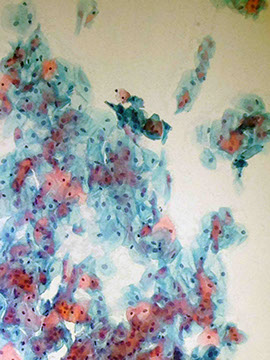
Squamous Metaplasia
Fragile columnar cells by tougher squamous cells at the squamo-columnar junction of endocervical canal
- the new squamous layer is more resistant to injury
- this kind of metaplasia can occur anywhere in the body with columnar epithelium
- often precedes or accompanies CIS
Characteristics:
- Poorly differentiated, sometimes dense cytoplasm
- Amphophilic stain that is very dense
- Active nuclei with smooth borders
- Pleomorphism
- Bizarre, single cells
- Small cells (in relation to normal squamous counterpart,
though the metaplastic cells can be pretty big)
- Variation of cell shape - cookie cutter / cobblestone arrangement
- cytoplasmic excrescence / tails
Most metaplastic groups look like endocervicals, but with
flattened, squamous-like cytoplasm
3 types of metaplasia:
1- Immature: looks like basal / parabasal cells c scant cytoplasm, round nucleus, finely granular chromatin present
2 - Mature: looks like parabasal to intermediate cell, but has more cytoplasm, some degenerative changes, moth bites, 2-toned cytoplasm, nuclear clearing, normal N:C ratio, cookie cutter cytoplasmic shape, more refractile, finely granular chromatin, spider-projections (little tails / pseudopods coming off of it)
3 - immature


Tubal Metaplasia
Columnar / cuboidal cells in small groups / pseudostratified
- round / oval enlarged pleomorphic hyperchromatic nuclei c evenly distributed chromatin
-- usually no nucleoli
Cytoplasm c vacuoles
Cilia / terminal bar often seen
- need to see > 1 cell to make the dx
Cells with cilia are generally benign (not 100%), here cells are tightly packed columnar cells with apical cilia


Dysplasia
Term meaning abnormal tissue growth
-Dyskeratosis is a term for the same on a cellular level
Follows metaplastic changes in the endocervical canal, and can either regress or progress to cancer
Characteristics of dysplasia in dyskeratotic cells are:
- Nuclear enlargement and irregularity (commonly see multinucleation)
- Hyperchromasia (bc have 2x the normal amount of chromatic present)
- Uniform, fine chromatin pattern
- may have chromocenters present
- Inc N:C ratio (small cells c large cytoplasms are bad)
- Pleomorphism
- Increased/decreased cell size
-Dyskeratosis
- Bizarre cells
Premalignant changes (refer to chart):
1. Rounded corners
2. Coarsely granular chromatin (can mimic layering of chromatin), perinuclear cavitation, and linear lying chromatin
3. Cauliflower cytoplasmic borders (vs right angle type)
HPV preferentially infects cells in the transformation zone (and is thus where CIN lesions begin)
Both the quantity and quality of the dysplasia matter!
Used to grade dysplasia:
- Mild dysplasia (CIN1): little inc in nuclear size, still finely granular and hyperchromatic chromatin, N:C ratio not really altered, pattern is slightly altered
- Moderate dysplasia (CIN2): Nuclear membrane starts to get more rounded
- Severe dysplasia (CIN3): Coarsely granular chromatin (hyperchromatic), N:C ratio very high, rounded borders, cloud-like nuclear membrane, single cells (loss of adhesion)
Loop Electrosurgical Excision Procedure (LEEP) used to tx CIN2/3
Carcinoma-in-situ (CIS): cytoplasmic membrane starts to drop out, syncytial grouping, not able to "walk" around nuclear membrane



Atypical Squamous Cells of Undetermined Significance (ASCUS)
MC squamous abnormality in Pap testing
- cells that are more atypical than just reactive cells, but not bad enough to be called malignant
Mildly enlarged nuclei (2-3x the size of the nucleus of an intermediate cell), smooth to slightly irregular nuclear membrane, mild hyperchromasia, uniform chromatin, no nucleoli
- N/C slightly inc
Can see HPV effects / binucleation, but not to the extent of LSIL
Pt should do HPV testing if >25 yo; if positive perform colposcopy
- for the pt <25 yo, repeat Pap smear in 12 mo c ASCUS
-- if Pap shows ASC-H, AGC, or HSIL in 12 mo, then should do colposcopy


ASC-H
Used when metaplastic or atrophic squames show some degree of atypia, but not possible to distinguish from HSIL
- can see sheets of <10 cells, usually sparse cells
- nuclei up to 2.5x that of immature metaplastic nucleus with smooth to slightly irregular nuclear membrane
- finely granular, evenly distributed chromatin
- has N/C close to that of HSIL
- nucleoli / chromocenters should be absent
Squamous lesions MC assoc HPV type 16


Carcinoma in Situ
By definition, is cancer that remains in the epithelial layer and has not spread past the basement membrane
- commonly occurs at the squamo-columnar junction from dysplastic / metaplastic cells
- DO NOT have nucleoli
On parafin embedded histologic sections the cells have loss of polarity and normal stratification (are jumbled and disorderly)
- appear crowded from loss of cytoplasm and affect the entire epithelial thickness, but do not invade past BM
- nuclei appear malignant, with course irregular chromatin and nuclear pleomorphism
Cytologically the cells can be singular or in aggregates, depending on the collection methods
- isolated cells more frequently seen when the endocervical canal or posterior vaginal fornix is sampled; aggregates (syncytial groups)more common when uterine cervix sampled
Endocervical CIS: overlapping nuclei, hyperchromasia of nuclei, elongated nuclei
Endocervical adenocarcinoma in situ: feathering of cytoplasmic border, elongated nuclei with hyperchromatic chromatin
- endocervical adenocarcinoma (not in situ anymore) will lose its feathering





LSIL
Nucleus 3-4x size of poly or intermediate cell nucleus and hyperchromatic, NO NUCLEOLI !!!
Smooth to slightly irregular nuclear membrane
Chromatin: slightly granular, evenly distributed
HPV features commonly seen: Sharp and irregular cavitation (in the cytoplasm??) c dense cytoplasmic rim, binucleation can be seen; N:C<50%
- <1% progress to cancer; but up to 25% have CIN2 or 3 upon biopsy
- sharp irregular cavitation can also be seen in koilocytes (can mimic navicular cells of pregnancy)
- chromatin can looked smudges c HPV effects
-- dx LSIL c HPV cytopathic changes if has dense peripheral rim of cytoplasm
Tx: Colposcopy done on pts >30 yo with LSIL with unknown HPV status or LSIL with + high-risk HPV
- if the pt is <24 yo, repeat Pap smear in 12 mo. 2/2 high-prevalence of HPV in this population and high rate of clearance of the virus
- colposcopy also performed on pts that are HIV+ and have dx of ASC-H, LSIL, HSIL, or SCC


HSIL
High N:C ratio (>50%)
Cells of parabasal size, assoc c HPV 16 and 18
Markedly irregular nuclear membrane (can be prominent) with frequent indentations / grooves that can make it look multi-dimensional
- ~1.5% progress to invasive ca, and ~75% show CIN2/3 on bx
- fine or coarse evenly-distributed chromatin sometimes witth clumping with hyperchromasia, scanty cytoplasm, though cytoplasmic borders can be pretty well defined
- some can be more uniformly round
- with a new dx of HSIL, must go back and review slides from the past 10 years
- may see Hyperchromatic Crowded Groups (HCGs) - sheets / syncytial groups (?) in loose clusters
-- groups of cells c irregular polarity
- no nucleoli visible
- isolated immature / abnormal squames can be a good clue to look closer for high-grade cells
Recommend LEEP or other tissue sampling
- colposcopy in adolescents and pregnants
DDx: normal endometrial cells, atrophy



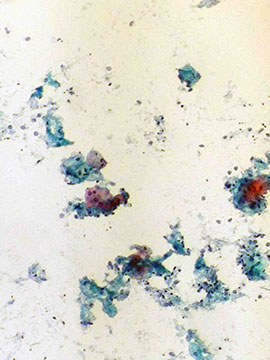
Squamous Cell Carcinoma
MCC (3/4) ca of cervix; pts 35-55 yo
Look for poorly differentiated single cells (or sometimes in syncytial groups) with prominent nucleoli and coarsely granular chromatin
- dyskeratotic cells with often be found too
Characteristics:
- Lage nucleoli present (though not as prominent as adenocarcinoma?), more common in NKSCC
- lots of single malignant cells
- Blood, inflammatory and degenerate (necrotic) background (tumor diathesis)
- Bizarre cells ("tadpoles" and fiber cells), elongated and orangeophilic
- Pleomorphism
- Dyskeratosis
- Abnormal keratinization
Should not be able to trace around the nucleus in most cases, nucleus should be irregular
Background of tumor diathesis can be seen
MC assoc c HPV type 16 (HPV type 18 MC in glandular lesions)
Tx: Excision, +/- chemoradiation





Glandular cells
From revised Bethesda 2001 Conference
Atypical Glandular Cells (AGC)
Endocervical, favor neoplastic
Morphologically almost reaches endocervical adenoca in situ / invasive
- cells in groups c nuclear crowding, overlapping, and poorly-defined borders
- nuclei enlarged and slightly hyperchromatic c coarse, very hyperchromatic chromatin
- inc N/C
- occasional mits
- high grade lesions found in 10-40% of these, but MC squamous and not glandular
Atypical Glandular Cells (AGC) - Endometrial, favor neoplastic
Cells in groups of 5-10 cells
Nuclei are slightly larger than those of normal endometrial cells c mild hyperchromasia, small nucleoli, scanty cytoplasm and ill-defined borders
Atypical Glandular Cells of Undetermined Significance (AGUS)
If first time dx, should repeat Pap smear at 1 year, preferably with HPV testing
-- if HPV is negative, then can repeat co-testing in 3 years
Adenocarcinoma in situ (AIS)
Precursor to endocervical adenoca; large groups of atypical cells
- often right next to adenoca in histo sections, but is rare to find
Abnormal architectural patterns maintained
- polarity c nuclei pointing towards outside of group
Nuclear crowding / stratification c hyperchromasia; crowding causes nuclei to become elongated; membrane usually smooth and regular; moderately cellular smear
- vacuolated cytoplasm c indistinct cell borders
- does NOT have cilia or terminal bars; no nucleoli either
Pseudostratification, "feathering"; Rosettes common, mits, crowding and strips; rarely see single cells
Nucleoli not present; NC ratio may be slightly increased
- mits present (not very frequent)
- no tumor diathesis
MC assoc c HPV type 18
- squamous lesions MC assoc c HPV type 16
- can have squamous and glandular lesions coexisting
Tx: Colposcopy
- bx if >35 yo or in younger pts c unexplained bleeding
Atypical Glandular Cells (AGC)

Adenocarcinoma in situ (AIS)

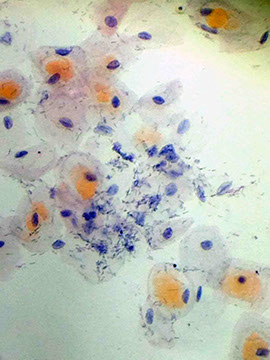
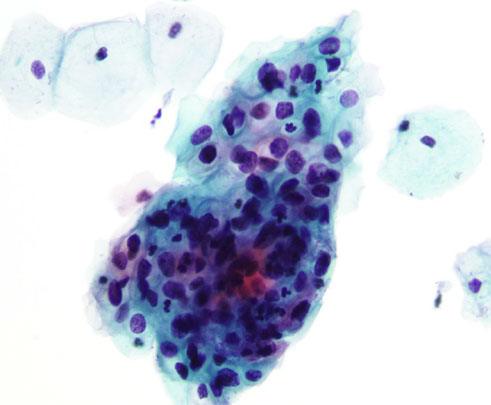
Endometrial adenocarcinoma
MC type of adenoca; the older the pt, the more likely it is endometrial
Characteristics:
- Prominent Macronucleoli that vary in number, size and shape
- Vacuolization (mucin vacuoles which may appear signet-ring) and PMN emperipolesis frequent
- Well-preserved glandular formations (balls, acini, papillary structures)
- syncytial groups (though usually single cells and small groups)
- delicate cytoplasm, Rounder shape
- usually hypOchromasia (not hyper), and nuclear membranes can appear thickened
- nuclear pleomorphism (SIZE! nucleus usually only about 1.5x that of poly)
Typically will see 3-D ball of cells that is apparent when focusing up and down
Macronucleoli are prominent and may be slightly eosinophilic, the nuclei should be 3-4x that of normal endometrial cells, estrogen will be elevated, nuclei eccentrically placed, mucin produced within cytoplasm, signet ring appearance
- phagocytosis of neutrophils helpful in dx'ing
- has more bloody background (vs inflam in endocervical adenoca)
Well-differentiated adenoca still has finely granular chromatin, but picket fencing lacking, overlapping nuclei, few prominent nucleoli (not very macro either), no mucin production
(+) Pancytokeratin, ER, Vimentin, and beta-catenin
Endocervical adenoca
Extremely rare and may have slightly larger cells than endometrial adenoca
- has eccentric, enlarged displaced nuclei, tags of cytoplasm, finely to slightly coarse hyperchromatic chromatin, fairly flat 2-D appearance forming microacini or rosettes or scalloping around the edges of the groups
- as it gets worse, the nuclei start to overlap, macronucleoli appear; but no matter how bad it gets, picket-fence will still be apparent
- multivacuolated cytoplasm c possible emperipolesis and has discreet cell borders
Prominent nuleoli, often multiple and irregular
(+) Pancytokeratin and p16
Reparative changes also in the ddx for adenoca (always look at the borders of the cell groups): nuclei have individual cytoplasmic membranes and the cytoplasm has pulled-taffy appearance
Ovarian adenoca may be seen and sheds big, classic vacuolated cells with prominent nucleoli
Adenosquamous ca: squamous component is mod to poorly differentiated to large cell NKSCC with endometrial adenoca component

Endometrial adenoca
Endometrial adenocarcinoma


Vaginal adenosis

Vaginal adenosis
DES causes multiple transition zones
- will see endocervical cells in a vaginal specimen
Clear cell carcinoma (of the vagina)
1/3 of the daughters with mothers exposed to DES develop vaginal adenosis (gland-formation in vaginal mucosa)
Clear cell carcinoma is the least common but worst common complication of in utero DES exposure
Small cell carcinoma
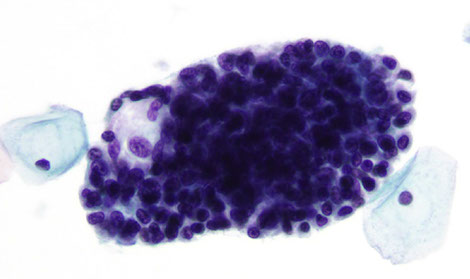
Clusters of small blue cells with hyperchromatic nuclei, scant cytoplasm, nuclear molding
assoc c HPV subtype 18
- resembles smal cell carcinoma of the lung
Similarly, is a very aggressive tumor assoc c distant mets
Culdocentesis / Ovarian Neoplasms
Overview
Ovarian ca responsible for ~20% of gynecologic malignancies
- important at the time of surgery
- precursor lesions (aka hyperplasia) not well defined
Normal cells should be medium-sized, have a central nucleus with consistent sizes, small nucleoli, delicate cytoplasm and vacuoles
- mesothelial cells in gutter washings appear to arrange in sheets and sometimes cluster together very tightly, sometimes looking more like endocervicals and endometrials
Reactive cells
Larger nucleus than normas, with denser chromatin than normal mesos
Atypical cells
Enlarged nuclei, occasional nucleoli, usually in sheets or small clusters
Cytologic difficulties arise with poor fixation, excessive staining of mesothelial cells, presence of single atypical mesothelial cells or macrophages, and arrangement of mesothelial cells in 3D papillary clusters
Differential diagnosis should include: poor fixation and excessive staining (cells stain dark and are hyperchromatic but nuclei are monotonous in size and configuration; cell clusters of papillary type are usually compact when compared with loosely arranged clusters of malignant cells; presence of psammoma bodies is controversial
*** if the tumor is grossly still confined to the ovaries, the presence of tumor cells in fluid aspirated from the cul de sac washings is of unfavorable, but by no means hopeless, prognostic significance
Suspect ovarian / tubal neoplasms with psammoma bodies found on Pap
