Effusions / Culdocentesis
Effusions
- General
- eosinophilic effusions
- Hematoxylin bodies
Mesothelial cells
Histiocytes
Atypical characteristics
Suspicious characteristics
Malignant characteristics
- mesothelioma
- Primary Effusion Lymphoma (PEL)
Peritoneal fluids
- serous tumors of ovary
Culdocentesis
Effusions
Malignancy causes exudates, thus transudates do not need to be evaluated for malignancy [?, 2]
Most effusions are benign (60-70%)
•Occasional non-malignant disease processes can be diagnosed via effusion cytology
About a third of effusions are malignant (30%)
•95% represent metastatic disease
•Initial presentation in 10-30% of patients with malignancy
•Documentation of tumor recurrence
•Poor prognosis for a malignant effusion (median <6 months survival)
•Role in tumor staging and treatment planning
•Molecular testing
- cytology better than blind bx to detect malignancy
- false-positive <1% [2]
- most malignant effusions already have a known primary tumor;
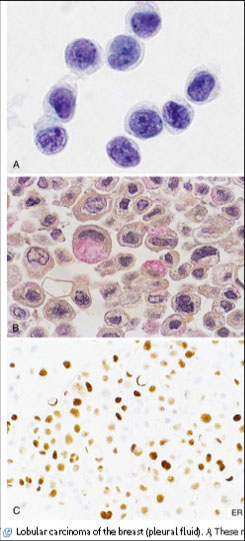
** MCC malignant effusion in men is lymphoma / leukemia, then GI / pancreatic ca; in
Features of Malignant Effusions
Increased cellularity
Numerous large clusters
Lacunae around tumor (Cell block sections)
Atypical cytomorphologic features
“Second population” - distinct from benign mesothelial cells
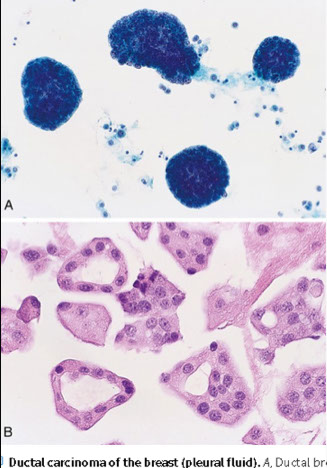
**in women is breast ca (CANON BALL!! [see image]), lung ca, lymphoma / leukemia
Eosinophilic effusions (eos>10%) MCC is pneumothorax / hemothorax; less commonly parasites, Churg-Strauss; 1/3 are idiopathic
Hematoxylin bodies:
***Remember***
Transudates: low specific gravity, low protein, low LDH
- exudates opposite
Mesothelial cells
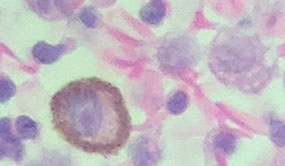
Fuzzy but definite cytoplasmic borders (the "skirt"), oval active central nuclei, possible multinucleation (esp 2 nuclei); denser cytoplasm, merging of several cells into small groups or a syncytial cluster
- 2 cells stuck together usually show a "window" caused by microvilli at outer rim of cytoplasm
- reactive mesos can have inc N/C, prominent (possible macro-)nucleoli, and some nuclear pleomorphism
- can form groups or papillary formations that look malignant, but should still have scalloped borders and windows
- looking outside of malignant looking groups for more benign / reactive cells can also be a clue that is b9
Histiocytes
Clear,delicate bubbly cytoplasm and greater tendency to form signet ring vacuolization than mesothelials; large NC ratio and typical central position of chromocenters
- nuclei less active than in mesothelial cells
Atypical characteristics
Defined as an effusion that is essentially normal with mesothelial alterations or atypia
- can be in a sheet-like arrangement or clusters, have prominent nucleoli, nuclear irregularities and enlarged nuclei
Suspicious characteristics
Defined as an effusion with cells suggestive of (but not conclusive for) malignancy
Rheumatoid Arthritis
Has multinucleated macrophages with an epithelioid population
Malignant characteristics
Primary cancers are rare, the most common types are malignant mesothelioma and primary effusion lymphoma
Papillary clusters (indicative of tumor implants), spherical clusters (sometimes called "morula" formations or proliferation spheres - a variant of the papillary cluster but highly suggestive of adeno, esp of the breast); dense nuclear branches (with scanty cytoplasm); enlarged nuclei (unusual inc in NC ratio); unusually large or elongated cells; Large red nucleoli; bizarre vacuolization (out of proportion to nuclear size); signet rings with molded nuclei; abnormal mitoses; sharp cellular borders; hyperchromasia
- lots of blood +/- lymphocytes usually is malignant
- NOT indicative of malignancy: loose aggregates (c irregular borders and windows); pairs of cells, usually mesothelials; single cells (unless obviously malignant or a lymphoma is in the ddx); multinucleated cells (usually histiocytes or mesothelial cells [binucleation is also common]); active nuclei (usually oval and centrally located); small dense nuclei (degenerate mesothelials and histiocytes); normal mitosis (fluid is a good growth medium); fuzzy rounded cytoplasmic edges
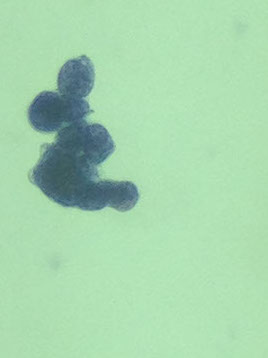
Squamous cell carcinoma
Central nuclei, nuclear pleomorphism, hyperchromatic to India ink chromatin, keratinized cytoplasm, and "tadpole" morphology

Mesothelial window
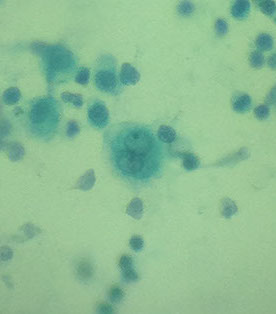
multinucleated meso

benign mesothelial cell cluster

reactive mesos

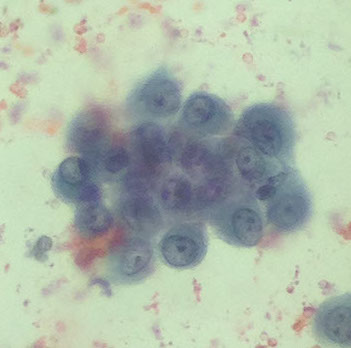
histiocyte cluster - peritoneal fl.

degenerating histiocytes

Adenoca
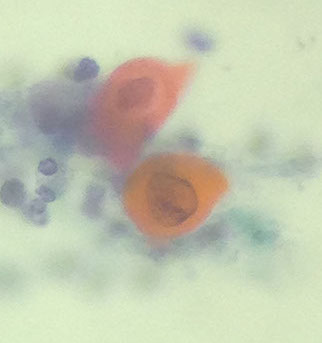
SCC
Immunoblastic lymphoma
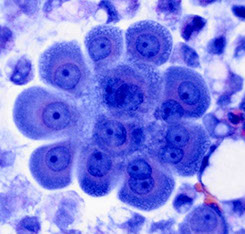
Mesothelioma
clustering of cells makes it at least suspicious for mesothelioma
- high NC, hypochromatic chromatin, macronucleoli, nuclear pleomorphism
- mesothelioma usually has more cells than adenoca
-- mesothelioma and adenoca have very distinct IHC
IHC (meso): (+) WT1, podoplanin (D2-40), calretinin
both adeno + meso , can be Moc-31 (+)!!
(+) for pankCK and neg vimentin
(+) EMA, neg desmin (b9 mesos have opposite staining)
- adenoca (+) for B72.3 and Moc-31
Definitive diagnosis generally requires evidence of invasion into skeletal muscle/adipose tissue on pleural biopsy
•Cannot prove invasion on cytologic effusion specimen!
3 main types:
1) Epithelioid: most common; most effusions
2) Biphasic
3) Sarcomatoid: rarely exfoliates
2 main patterns:
1) Large clusters with scalloped borders (“mulberry clusters”)
- “Windows” and “lacy skirts” like normal mesothelials
- Clusters of >20-40 cells are indicative of malignancy
2) Numerous dyshesive cells
- “Mesothelial morphology” but with severe cytologic atypia
- Diagnostically challenging
Often need ancillary studies.
Genes: Homozygous 9p21 deletion has 100% specificity
• p16/CDKN2A tumor suppressor gene
- ~80% of mesotheliomas have some kind of alteration to the BAP-1 gene, which correlates c a loss of IHC expression
In Primary Effusion Lymphoma (PEL), see large dispersed cells, round irreg nucleus, prom nucleoli, lots of basophilic cytoplasm (cells are very weird)
- usually in immunocomp pts
- (+) HHV-8, CD45/30/38/138; negative CD19/20
Malignant Mesothelioma


Mesothelioma
Melanoma
Single cells c eccentric nuclei, prominent nucleoli and melanin pigment in cytoplasm
- amelanotic melanoma characteristically has a refractile clearing in the nucleus

Melanoma
Peritoneal fluid
Serous tumors of the ovary
Difference bwt borderline and malignant tumor is stromal invasion
- see relatively small cells singly or in small papillary clusters that are uniform c high N/C ratio and possibly a little bit of cytoplasmic vacuolization, commonly psammoma bodies
- finding tumor in peritoneal washing upgrades from a stage Ia/b to a stage Ic
Tx: postop chemo has no survival advantage
Px: pretty good even without adjuvant chemo
Anaplastic Small Cell Carcinoma
Small clusters / sheets of hyperchromatic cells c nuclear pleomorphism, molding and crush artifact
Relatively rare: Pleural effusions in <3% of patients with SCC; Smoking history; Can be subtle (IHC)
Cytologic features: Small clusters/individual cells, Less molding/angulated nuclei in LBPs, Single cell apoptosis; Mitotic activity
Pseudomyxoma Peritonei
Mucinous tumor that surrounds peritoneal organs
- background can have some columnar cells c irreg fragments of thick basophilic mucous

Small cell ca
Culdocentesis
Cul-de-sac aspiration via vaginal route to dx early clinically occult ovarian cancers (ovarian ca is ~20% of all malignant tumors)
- surgeon aspirates any fluid present and washes out the cul de sac with saline
Mesothelial cells
Medium-sized, central nuclei c consistent size, usually have small nucleoli, delicate cytoplasm and vacuoles
- may appear bad c poor fixation, excessive staining of mesothelial cells, presence of single atypical mesothelial cells or macrophages, arrangement of mesothelial cells in 3D papillary clusters
Atypical cells
Enlarged nuclei, nucleoli occasionally seen, usually in small sheets or clusters
References
1. Notes, the U
2. Cibas. Cytology. Next ed to the new one. Ch 4
